See: Article 1: Practical tips in the assessment of chronic spontaneous urticaria (CSU), March 21, 2023
Authors
Kevin KD Lee, MD, FRCPC (biography and disclosures)
Disclosures: Received resident research funding from ImmUnity Canada (previously known as Canadian Immunodeficiencies Patient Organization). Mitigating potential bias: Recommendations are consistent with published European and Canadian guidelines and with current practice patterns. Only published trial data are presented. Treatments or recommendations in this article are unrelated to the research grant from the disclosure statement.
Persia Pourshahnazari, MD, FRCPC (biography and disclosures)
Disclosures: Received honoraria for speaking engagements from Octapharma, Takeda, CSL Behring, Stallergenes Greer, Novartis, and Astra Zeneca. Advisory board member for Octapharma, Takeda, CSL Behring, Novartis, Astra Zeneca, Valeo, Bausch Health, Sanofi, and Aralez. Mitigating potential bias: Recommendations are consistent with published European and Canadian guidelines and with current practice patterns. Only published trial data are presented.
What frequently asked questions we have noticed
Chronic spontaneous urticaria (CSU) is a common condition that is seen in both primary and specialty care practices.1,2 While not a fundamentally dangerous condition, CSU can have a significant impact on patients’ quality of life and can be challenging to manage. Symptoms can be prolonged and can recur even after a long symptom-free period.1,2 Our local experience has identified some frequently asked questions around the management of CSU, namely on the use of antihistamines (including optimal dosing, duration, tapering methods, and antihistamine use in special populations). This is the second of two articles aimed at providing answers to the above questions based on the recently updated 2022 European position statement on CSU and the 2018 Canadian practical guide on chronic spontaneous urticaria.1,2
Data that answers these questions
What are the recommended treatments for CSU?
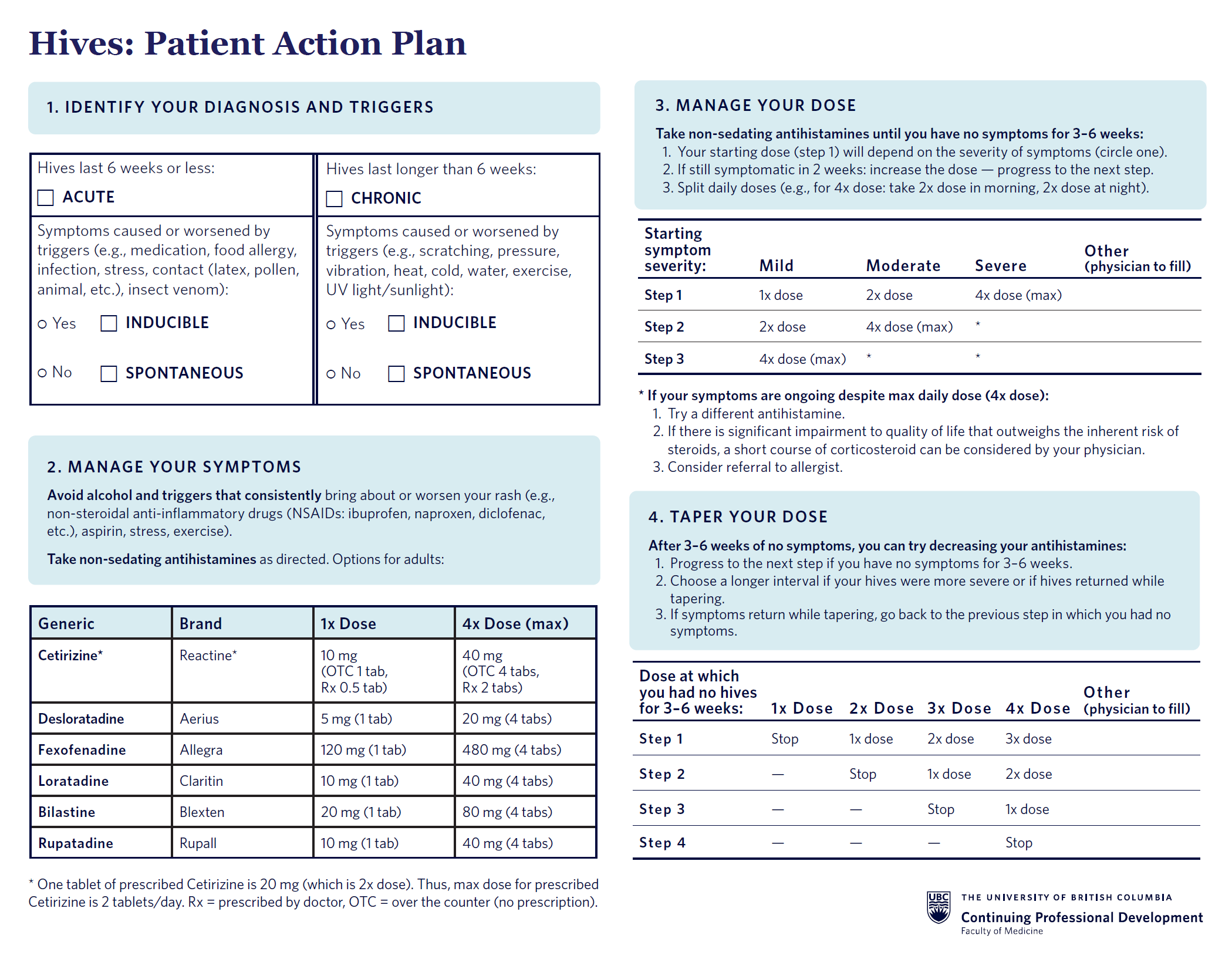
The recommended first-line therapy for CSU is non-sedating H1-antihistamines, of which there are several available choices (Table 1).1,2 The choice of medication used may be made based on cost, availability, and patient preference. If one agent is not effective, then other antihistamines can be tried next. In our local practice, daily antihistamine use is recommended rather than on-demand treatment. This is because significant quality-of-life improvements were noted with regular daily use in previous studies.3,4 Consistent with the 2022 European position statement and the 2018 Canadian practical guideline, we recommend using the lowest dose of non-sedating H1-antihistamine that ameliorates symptoms.1,2 Dose escalation, up to fourfold the routine daily dosage, can be tried next if symptoms are not well-controlled. A sample schedule is provided in Table 2.
Short courses of systemic corticosteroids can be added for management of severe urticaria. While there are no specific criteria for when to start corticosteroids for severe urticaria, the local practice pattern is to start when the quality of life is significantly impaired by urticaria and the benefit of treatment with prednisone outweighs the inherent risk of corticosteroids (e.g., hyperglycemia, weight gain, infection risk, etc.). A routine regimen would include prednisone 0.3 to 0.5 mg/kg for 1–2 weeks followed by a slow taper.
Of note, first-generation H1-antihistamines (e.g., diphenhydramine, hydroxyzine) are no longer recommended for management of CSU. This is due to an unfavorable adverse effect profile including sedation, cognitive impairment, and psychomotor impairment. These drugs also have a shorter duration of action compared to second and third-generation non-sedating antihistamines.5
Table 1. Adult Doses for Non-Sedating H1-Antihistamines (download)
| Generic | Cetirizine | Desloratadine | Fexofenadine | Loratadine | Bilastine | Rupatadine |
| Brand | Reactine | Aerius | Allegra | Claritin | Blexten | Rupall |
| 1x Dose | 10 mg | 5 mg | 120 mg | 10 mg | 20 mg | 10 mg |
| 4x Dose (max daily) | 40 mg | 20 mg | 480 mg | 40 mg | 80 mg | 40 mg |
| Pharmaceutical options: | ||||||
| Tablet (mg/tablet) | OTC: 10 Rx: 20 |
5 | 120 | 10 | 20 | 10 |
| Dissolvable tablet (mg/tablet) | 10 | — | — | 10 | 10 | — |
| Liquid (mg/mL) | 1 | 0.5 | — | 1 | 2.5 | 1 |
| Other notes: | ||||||
| Availability | OTC, Rx* | OTC | OTC | OTC | Rx | Rx |
| * Note dose differences between OTC and Rx tablets. OTC: Over-the-counter. Rx: Prescribed. | ||||||
Refer to product monographs for pediatric dosing.
Table 2. Sample Daily Dose Escalation Schedule for Non-Sedating H1-Antihistamines (download)
| Starting symptom severity: | Mild | Moderate | Severe |
| Step 1 (initial dose) | 1x dose | 2x dose | 4x dose (max) |
| Step 2 | 2x dose | 4x dose (max) | * |
| Step 3 | 4x dose (max) | * | * |
Patient instructions:
* If symptoms are ongoing despite maximal daily dose (4x dose daily):
Example: Suppose a patient reports moderate quality of life impairment (middle column). In this case, use the column labeled “Moderate” to dose-escalate. Start at Step 1 (2x dose daily). If the patient still has symptoms after 2 weeks, increase to Step 2 (4x dose daily). If they still have symptoms after 2 weeks, they could consider switching antihistamines, adding corticosteroids, and/or referral to an allergist. |
|||
How long can antihistamines be used for?
A recent, multi-centre, real-life pilot study assessed the efficacy and safety of long-term and high-dose antihistamines in patients with CSU.6 The average duration of therapy was 24 weeks. 7.9% (11/139) of patients experienced side effects at standard dosing (1x dose) while 5.2% (5/96) experienced side effects at higher doses. The most common side effect was somnolence; other infrequent side effects included headache, diarrhea, thirst, and hand numbness. Review of other studies by the European position statement also did not note any serious adverse effects at higher doses for long durations.1 As such, our local practice does not limit the duration of therapy.
How should antihistamines be stopped?
To our knowledge, there is no specific recommended tapering schedule for antihistamines. The following tapering plan (Table 3) could be tried as per local practice patterns after patients have had no symptoms for at least 3 to 6 weeks while on the current dose of antihistamines. If symptoms recur during tapering, then the patient should return to the previous dose at which they had no symptoms.
Table 3. Sample Tapering Scheduled of Non-Sedating H1-Antihistamines (download)
| Dose without urticaria for 3–6 weeks | 1x Dose | 2x Dose | 3x Dose | 4x Dose |
| Step 1 | Stop | 1x dose | 2x dose | 3x dose |
| Step 2 | — | Stop | 1x dose | 2x dose |
| Step 3 | — | — | Stop | 1x dose |
| Step 4 | — | — | — | Stop |
Patient instructions:
Example: Suppose a patient is on 3x dose daily and is symptom-free for at least 3 weeks on this dose. Discussion should be made with patient to consider dose reduction using the column labeled as “3x Dose”. Ask the patient to decrease to Step 1 (2x dose daily). If no symptoms for at least 3 weeks, decrease to Step 2 (1x dose daily). If no symptoms for at least 3 weeks, decrease to Step 3 (Stop). However, if urticaria recurs (e.g., while on Step 3), they would return to the previous step (e.g., back to Step 2). |
||||
Are there any recommendations for special populations?
The recommendations below are based on the 2022 European publication.1
- Pediatric: There is no change in the above management guideline other than to ensure that the 1x dose is at a pediatric dose.
- Pregnancy: Loratadine is the preferred non-sedating H1-antihistamine in pregnancy as it has the largest metanalysis safety data. Cetirizine and desloratadine can also be used, although sample sizes are smaller. However, studies with doses higher than 1x dose are limited and should be used with caution.
- Breastfeeding: While considered to be safe, all H1-antihistamines are secreted into breast milk. As such, non-sedating H1-antihistamines are recommended due to their minimal side-effect profile.
When should a specialist referral be made?
While referral to an allergist for urticaria can be made at any time, health-care providers should particularly consider a referral if urticaria is persistent or not responsive to maximally up-dosed non-sedating antihistamines. These patients would be considered for escalation of therapy with omalizumab or cyclosporin which is beyond the scope of this article. Other reasons for referral may include suspected cases of inducible urticaria for further investigation and management, and for possible true IgE-mediated allergy or anaphylaxis.
What we recommend (practice tips)
For the management of CSU, we summarize the above discussions as follows:
- The management goal of CSU is the complete remission of symptoms.
- Daily use of non-sedating H1 antihistamines is recommended as compared to on-demand treatment.
- Non-sedating antihistamines can be safely titrated up to fourfold the typical daily dosage and can be used for as long as they are needed.
- For ease of prescribing, you can write the following non-sedating antihistamine options for adults into your EMR. For patient instruction, consider adding “Use every day as per the escalation and tapering table” to the prescription so that patients remember to use it regularly rather than only when there is a rash.
- Cetirizine 10–20 mg PO BID PRN
- Bilastine 20–40 mg PO BID PRN
- Rupatadine 10–20mg PO BID PRN
- Desloratadine 5–10 mg PO BID PRN (Note, this is over-the-counter)
- Fexofenadine 120–240 mg PO BID PRN (Note, this is over-the-counter)
- Loratadine 10–20 mg PO BID PRN
- Preferred non-sedating antihistamines for pregnant individuals include loratadine, cetirizine, or desloratadine.
- First-generation H1-antihistamines (e.g., diphenhydramine, hydroxyzine) are no longer recommended due to unfavorable adverse effect profiles.
Handout for patients
References
- Zuberbier T, Aberer W, Asero R, et al. The EAACI/GA²LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy. 2018;73(7):1393-1414. doi:10.1111/all.13397 (View)
- Kanani A, Betschel SD, Warrington R. Urticaria and angioedema. Allergy Asthma Clin Immunol. 2018;14 (Suppl 2):59. Published 2018 Sep 12. doi:10.1186/s13223-018-0288-z (View)
- Grob JJ, Auquier P, Dreyfus I, Ortonne JP. How to prescribe antihistamines for chronic idiopathic urticaria: desloratadine daily vs PRN and quality of life. Allergy. 2009;64(4):605-612. doi:10.1111/j.1398-9995.2008.01913.x (Request with CPSBC or view with UBC)
- Weller K, Ardelean E, Scholz E, Martus P, Zuberbier T, Maurer M. Can on-demand non-sedating antihistamines improve urticaria symptoms? A double-blind, randomized, single-dose study. Acta Derm Venereol. 2013;93(2):168-174. doi:10.2340/00015555-1434 (View with CPSBC or UBC)
- Fein MN, Fischer DA, O’Keefe AW, Sussman GL. CSACI position statement: Newer generation H1-antihistamines are safer than first-generation H1-antihistamines and should be the first-line antihistamines for the treatment of allergic rhinitis and urticaria. Allergy Asthma Clin Immunol. 2019;15:61. doi:10.1186/s13223-019-0375-9 (View)
- Zhang L, Wu J, Qi Y, et al. Long-term combinations and updosing of second-generation H1-antihistamines show efficacy and safety in the treatment of chronic spontaneous urticaria: A multicenter real-life pilot study. J Allergy Clin Immunol Pract. 2020;8(5):1733-1736.e11. doi:10.1016/j.jaip.2019.12.006 (Request with CPSBC or view with UBC)

Excellent Information! Thank you.
Does the “4x dose” refer to the total daily dose of the relevant antihistamine? So for cetirizine it would be 40mg daily or 20mg BID?
Hi Sonja Babovic,
4x refers to the maximum dose that patients could take within 24 hours, with 1x referring to a single tablet dose (the exception is for prescribed Cetirizine which comes in 20 mg tablets (instead of 10 mg per tablet over the counter)).
As such, 4x would still be 40 mg for Cetirizine. However, it would be 4 tablets for OTC and 2 tablets for Prescribed. Either option is fine to use. We generally use prescribed Cetirizine (rather than OTC Cetirizine) if they have drug coverage.
For all options, the total daily dosing can be split throughout the day based on patient preference.
As someone who’s experienced CSU I can attest to the negative impact it can have on quality of life. I think it would be great to do a follow up on this to review family physician role in prescribing omalizumab. I think this could be within the scope fo family practice when appointments with allergists are hard to come by.
Do you see any role for H2 receptor antagonists?
Or montelukast?
Thank you for this great article!
Can up dosing of Blexten (Bilastine) be done if 20mg is prescribed alongside a 5 day course of 40mg prednisone?