Shari Hurst, RN BN (biography, no disclosures) Disclosures: No disclosures. Only published trial data is presented. Recommendations are consistent with published guidelines from Canadian Cardiovascular Society 2021. Recommendations are consistent with current practice patterns.
Frequently asked questions
Canadian Cardiovascular Society (CCS) guidelines inform clinicians on how to initiate and titrate optimal medical therapy for heart failure with reduced ejection fraction (HFrEF) of 40% or less. In 2021, updated HFrEF guidelines include comprehensive, or foundational, therapy from 4 classes of medications:
- ARNI (sacubitril/valsartan, in place of ACEI/ARB for further reduction in CV death, hospitalizations, and symptoms)
- Beta-blocker (bisoprolol, carvedilol)
- MRA (spironolactone, eplerenone)
- SGLT2 inhibitor (dapagliflozin, empagliflozin for patients with or without diabetes to reduce HF hospitalizations, improve survival and HF symptoms)
(McDonald, Virani, et al, 2021)
Furthermore, CCS recommends foundational therapy be initiated and titrated to maximum tolerated target doses within 3–6 months. Given the complexity of the HF therapies and HF patient population, foundational therapy has brought forward questions from health care providers:
- How can I support my patients to tolerate HFrEF medical therapy?
- How can I support my patients to adhere to HFrEF medical therapy?
- How do I support my patients with self-management strategies?
Data that addresses these questions
How to initiate/uptitrate HF medical therapy
Previously, HF therapies would be initiated and up-titrated in a step-wise plan with one drug class at a time. In 2021 CCS recommended initiation and uptitration of HF therapies in a “cluster” style, to maximize early survival benefits. The following algorithm illustrates HFrEF treatment plan: view. Or view here: The Canadian Cardiovascular Society. Is it heart failure and what should I do — 2021 Update — Pocket guide. Pg 14. (View)
McMurray and Packer (2021) have proposed an algorithm on how to start the foundational 4 in a cluster style:
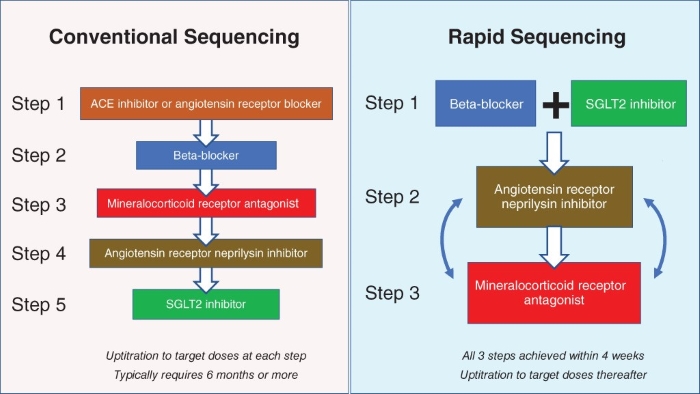
Packer M, McMurray JJV. Rapid evidence-based sequencing of foundational drugs for heart failure and a reduced ejection fraction. Eur J Heart Fail. 2021 Jun;23(6):882-894. *Corresponding author. Baylor Heart and Vascular Institute, 621N. Hall Street, Dallas, TX 75226, USA. Tel:+1214 820-7500, Email: milton.packer@baylorhealth.edu. Open access article under the terms of the Creative Commons Attribution-NonCommercial License.
Special considerations:
- When titrating ACE/ARB/ARNI, MRA, SGLT2i, and diuretics, check electrolytes, creatinine GFR in 7–10 days. Up to 30% decline in renal function is considered acceptable. Potassium level up to 5.5 mmol/L is considered acceptable.
- ARNI is preferred over ACE/ARB. BC Pharma Care coverage for ARNI is limited to cardiology or internal medicine to prescribe on initiation and 4-week trial of ACE or ARB before Special Authority for ARNI will be approved: view at gov.bc.ca.
- When converting from ACEi: Stop ACEi, wait at least 36 h after last dose (increased risk of angioedema), then start ARNI. Washout is not required for ARB, start ARNI when next dose would have been due.
- SGLT2 inhibitors offer cardio and renal protection. As of January 2022, BC Pharma Care Special Authority is now available for dapagliflozin for HF indication: view at gov.bc.ca. Approval requires adjunctive treatment with beta-blocker, ACE/ARB/ARNI and MRA unless contraindicated.
- To help guide decision-making regarding the addition of SGLT2 inhibitors, the Canadian Heart Failure Society (CHFS) has created an algorithm for prescribing SGLT2i inhibitors: view.
- Reference tool for starting doses of medications, preferred HF ACE/ARB, beta-blockers, MRA, when to repeat blood work can be found at: view at Canadian Cardiovascular Society ccs.ca.
- Further information regarding CCS guidelines, treatment algorithm, and medication sequencing, supporting research trials can be found at: CCS.ca/eguidelines
How to support patients
Multiple studies have shown that a focus on patient education and empowerment along with clinical follow-up for HFrEF medical treatment improves survival, reduces hospitalizations, and improves quality of life (Virani et al, 2017). HeartLife Foundation’s Patient & Caregiver Charter of Rights underscores the burden of HF on patients and their caregivers, as well as patients’ right to access timely, empathetic, evidence-based care that includes tools to empower their individual ability to participate in their health care (HeartLife, 2021).
What I recommend (practice tip)
There are a few tips and tricks to improve medication tolerance and adherence, and improve quality of life for patients with HFrEF.
Supporting tolerance of optimal HFrEF medical therapy
The combined effects of ARNI, MRA, and SGLT2i at promoting naturesis and diuresis help to reduce volume overload in HF, allowing for reduction or cessation of diuretics. This opportunity can present itself as postural hypotension, feeling lightheaded or dizzy, a drop in home weights, and/or a >30% decline in renal function and elevated potassium on follow-up blood work. Tips to manage these effects are:
Blood pressure effects
There is no target blood pressure for HFrEF. Asymptomatic BP of less than 100 mmHg systolic is acceptable. Check orthostatic BP readings to identify patients at risk of symptomatic hypotension. If concerned:
- Always assess for euvolemia prior to reducing HF meds due to postural hypotension. Often reducing/stopping diuretics, or liberating patients from fluid restrictions resolves symptoms.
- Consider staggering doses of beta-blocker and ARNI to reduce BP-lowering effects
- If the patient is on carvedilol, consider switching to bisoprolol (more beta-selective, once a day at bedtime dosing).
Renal effects
A slight renal decline up to 30% is acceptable with initiation and titration of ARNI/ACE/ARB, MRA, SGLT2i. If concerned about decline in renal function:
- Assess for euvolemia. Is it possible to reduce diuretics & keep cardioprotective HF med?
- It is important to counsel patients about sick days. Dehydrating illnesses can lead to AKI, trips to ER, and reduction of HF meds. SADMANS is one mnemonic to guide prescribers about holding medications (View, pg 2).
- Repeat electrolytes, creatinine 7-10 days after dose titration.
Potassium effects
Several HFrEF medications can increase potassium levels. Most often, mild hyperkalemia can be resolved with dietary modifications.
- A potassium up to 5.5 mmo/L is acceptable.
- Prior to reducing HFrEF meds, assess for euvolemia. Often hyperkalemia accompanies rise in creatinine and drop in GFR. This may be an indication of volume depletion, and an opportunity to reduce/stop diuretics.
- If not on diuretics, encourage increase in fluid intake for mild hyperkalemia, then re-check renal function and electrolytes.
- Patient resources outlining high/low potassium foods can be found on the Cardiac Services BC website: view.
Supporting HFrEF medication adherence
Present HF medications as an opportunity to feel better and live longer with HF to help establish a positive mindset when initiating/up-titrating doses.
- Write down medication directions in plain language — i.e. take 1 tablet, morning and evening.
- Patient information sheets for HF medications can be found on the Cardiac Services BC website: view.
- Ensure patients have applied for Fair PharmaCare so eligible drug costs will be supported by provincial coverage: view.
- Write on the prescription that the Special Authority has been sent for applicable drugs. Then ensure it is sent in! They are not retroactive, so monies spent prior to approval will not be applied to annual deductible (and not covered by PharmaCare!)
- Blue Cross has a website called Pharmacy Compass which lists medication costs and dispensing fees by pharmacy: view.
- Some patients will need support filling out PharmaCare forms; involve caregivers in medication discussion or engage social work support
Supporting HF self-management
Recognizing a change in HF can be tricky for some patients. HF is often accompanied by multiple co-morbidities, each with their own clinical picture, creating a constellation of symptoms and further complexity to recognize and appropriately respond to changes. Some strategies to manage this challenge are:
- Use the Heart Failure Zones as a resource for identifying and monitoring HF symptoms.
- Personalize Heart Failure Zone information. Ask patients to “star” the symptoms they remember having when first diagnosed with HF as a reminder of what symptoms they might first notice if their condition changes. It is available in multiple languages on the Cardiac Services BC website: view.
- Encourage use of a daily weight chart with emphasis on what patients are to monitor: weight gain of 4 pounds in 2 days or 5 pounds in a week. Include a reminder to limit sodium and fluid intake. Daily weight resources can be found at the Cardiac Services BC website: view.
- If HF symptoms do change, who should patients call? Write down the contact information.
- When patients do call, thank them for checking in. Reinforce efforts at every opportunity — “I’m so glad you called about…”
- Use problem-solving and experiential learning versus blame to help prevent feelings of guilt — “What do you think happened?”
- Engage family members/support person to support medication adherence and self-monitoring.
- Don’t be afraid of internet searches, but rather confirm what they have learned or offer alternate website resources to read.
Resources
- Cardiac Services BC has fantastic HF resources including pamphlets and videos. They can be found at: Cardiacbc.ca.
- Heart and Stroke Canada has adopted many BC resources and offers some resources in multiple languages as well as free booklet “Living Well with Heart Failure” which contains most resources. (View)
- Canadian Heart Failure Society has up-to-date HF provider information such as the SGLT2 inhibitor algorithm, educational materials, and learning opportunities as well as patient resources: heartfailure.ca.
- HeartLife Foundation is a national patient-led organization aimed at raising awareness, support, and advocating for better HF care for all: heartlife.ca. They have also developed a patient support app and learning website HeartLife.Academy to support patient knowledge about their HF.
References
- Packer M, McMurray JJV. Rapid evidence-based sequencing of foundational drugs for heart failure and a reduced ejection fraction. Eur J Heart Fail. 2021 Jun;23(6):882-894.
- Alpert CM, Smith MA, Hummel SL, Hummel EK. Symptom burden in heart failure: assessment, impact on outcomes, and management. Heart Failure Rev. 2017; 22(1): 25-39. DOI: 10.1007/s10741-016-9581-4. (View)
- Canadian Heart Failure Society. Practical Approach to SGLT2 inhibitors for treatment of cardiovascular disease. 2020. (View)
- Heart Failure. Cardiac Services BC. Accessed Jan 6, 2022 (View)
- Fonarow GC, Albert NM, Curtis AB, et al. Improving evidence-based care for heart failure in outpatient cardiology practices: primary results of the Registry to Improve the Use of Evidence-Based Heart Failure Therapies in the Outpatient Setting (IMPROVE HF). Circulation, 2010;122(6): 585-596. DOI: 10.1161/CIRCULATIONAHA.109.934471. (View)
- Heart Failure. Heart and Stroke Foundation. Accessed Jan 6, 2022 (View).
- HeartLife Foundation. Patient Journey Map. October 2021. (View)
- HeartLife Foundation. Canadian Heart Failure Patient & Caregiver Charter. 2021. (View).
- Howlett JG, Chan M, Ezekowitz JA, et al. The Canadian Cardiovascular Society Heart Failure Companion: Bridging Guidelines to Your Practice. Can J Cardiol. 2016;32(3):296-310. DOI: 10.1016/j.cjca.2015.06.019. (View with CPSBC or UBC)
- Ezekowitz JA, O’Meara E, McDonald MA, et al. 2017 comprehensive update of the Canadian cardiovascular society guidelines for the management of heart failure. Can J Cardiol. 2017;33(11):1342-433. DOI: 10.1016/j.cjca.2017.08.022. (View with CPSBC or UBC)
- McDonald M, Virani S, Chan M, et al. CCS/CHFS Heart Failure Guidelines Update: Defining a New Pharmacologic Standard of Care for Heart Failure With Reduced Ejection Fraction. Can J Cardiol. 2021;37(4):531-46. DOI: 10.1016/j.cjca.2021.01.017. (View).
- Virani S, Bains M, Code J, et al. The Need for heart Failure Advocacy in Canada. Can J Cardiol. 2017;33(11):1450-4. DOI: 10.1016/j.cjca.2017.08.024. (View)

Good article, but I found this portion of it patronizing:
When patients do call, thank them for checking in. Reinforce efforts at every opportunity — “I’m so glad you called about…”
Use problem-solving and experiential learning versus blame to help prevent feelings of guilt — “What do you think happened?”
Engage family members/support person to support medication adherence and self-monitoring.
Don’t be afraid of internet searches, but rather confirm what they have learned or offer alternate website resource
Very easy to follow algorithm. In reality, our prescribing practice is somewhat dictated by what medication Pharmacare will cover.