Dr. Jennifer Grant (biography and disclosures) Disclosures: Research grants and funding from Accelerate diagnostics. Relationship with a not-for-profit agency: Association of Medical Microbiology and Infectious Disease Canada. Mitigating Potential Bias: I do NOT have any affiliations (financial or otherwise) with commercial organizations. I am passionately engaged in the work of antimicrobial stewardship. I participate in several provincial and national groups that contribute to the knowledge base of stewardship. This work is intended to be for the common good and does not benefit me personally. The content of this article are evidence based and intended to advance better antimicrobial prescribing.
What I did before
I was trained as a resident to always ask about a patient’s allergies and to never use similar medications. This was thought to be the best way to protect patients from possible adverse reactions – and physicians from legal action. Any reaction self-described as an allergy was thought sufficient to stop using that class of drug, “just in case.” The rule, in particular, is applied to penicillin-like antibiotics given their potential for severe allergic reactions and cross reactivity within the class. Therefore, for any patient who reported an allergy to any beta-lactam, I would always prescribe non beta-lactam antibiotics for these patients, just to be safe.
While this is generally considered the “safe” thing to do, there are a number of down-sides. The first is the relative ineffectiveness of other antibiotics. Beta-lactams when compared head-to-head against almost any other class of drug on susceptible organisms have superior efficacy. In addition the class usually portends a lower toxicity and a greater therapeutic window. For example, the quinolones are associated with cardiac and connective tissue toxicity (there is a FDA black-box warning against their use for minor infections), aminoglycosides are nephro- and oto-toxic, Trimethoprim-sulfamethozole has significant bone-marrow toxicity. There is also evidence that agents like the quinolones are more likely to cause organisms to express resistance.[i] For example at my hospital our current resistance of E. coli to third generation ceaphlosporins is 13% while the resistance to quinolones is 22%. For empiric therapy therefore there is a significant risk to using non-beta-lactam antibiotics.
What changed my practice
Recent data show that up to 90% of patients with a reported penicillin allergy are mislabelled and of those who are allergic, many beta-lactams can still be safely prescribed due to low risk of cross-reactivity. Mislabelling of penicillin allergy is due to many things including misdiagnosis (confusing a viral exanthema for allergy), purer formulations of antibiotics, loss of allergy and differences in side-chain structure. For example, Cefazolin does not share side-chains with most penicillins and thus can be safely used for surgical prophylaxis in many penicillin allergic patients. This knowledge combined with the fact that beta-lactams remain one of the most effective and least toxic class of antibiotics has caused me to act to remove penicillin allergies in every patient I can.
What I do now
The most important thing in addressing a patient with a history of beta-lactam allergy is to ask the patient’s history of allergy to assess the true risk — to know when to ignore an allergy history and when further testing is recommended. For example, nausea, diarrhea or headache are predictable side effects of antibiotics, certainly unpleasant for the patient, but they are not allergies. There are also a number of patients who had a reaction that may have been allergic, but they have subsequently used the same class of antibiotics without an adverse event, suggesting their previous reaction either wasn’t an allergy, or that the allergy is no longer present. Severe reactions however, are a reason for even more careful history taking, as some adverse events are life threatening, but may not be classified as an allergy. Bone marrow suppression and Stevens-Johnson Syndrome are the most feared adverse events associated with beta-lactam use and should make a clinician very circumspect about considering these agents without expert consultation.
My history of a patient with a beta-lactam allergy includes the following information: 1. What was your reaction exactly 2. Did you need medical attention for the reaction, if so, what? 3. Do you remember which specific drug caused the reaction 4. When did this reaction happen 5. Have you taken any penicillins since then (I often name a number of drugs – I also check with the patient’s pharmacy and GP)
These questions allow me to assess the timing and severity of the reaction – the milder the reaction and the longer the period since the reaction, the less likely the patient is to react again. Particularly severe reactions; those that required hospitalization or other medical attention, I will refer for skin testing or allergist opinion. Knowing the specific drug, especially for mild reactions, allows one to avoid that specific drug or drugs with similar side-chains (the more common cause of reaction for cephalosporins). Additionally knowing that the patient has already taken the same class without reaction is reassuring that the “allergy” was likely attributable to other causes or has abated. There are numerous clinical algorithms that help prescribers use this information to make decisions about removing the allergy, further testing or confirming the allergy.
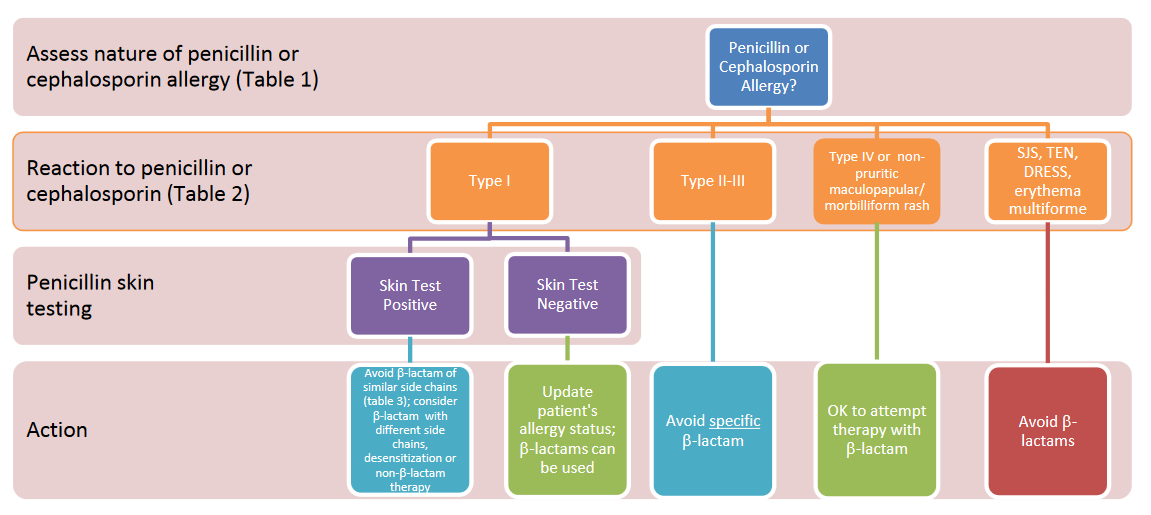
Resource #4: Beta Lactam Allergy Algorithm. Provided with permission from Dr. Cesilia Nishi. Full handout: http://bit.ly/TCMPBLAa. Adapted from Adapted from Antimicrobial Treatment Guidelines for Common Infections. The NB Provincial Health Authorities Anti-infective Stewardship Committee. June 2016.
Resources and Handouts:
- Providence Health Care Algorithm “Antimicrobial – cephalosporin use in penicillin allergic patients” https://thischangedmypractice.com/Antimicrobial-Use-Penicillin-Allergy. Provided with permission from Dr. Victor Leung, The Providence Health Care (PHC) Antimicrobial Stewardship Program (ASP). Accessed July 18, 2017. (View)
- National Center for Emerging and Zoonotic Infectious Diseases Division of Healthcare Quality Promotion. Is it Really a Penicillin Allergy? Evaluation and Diagnosis of Penicillin Allergy for Healthcare Professionals. Accessed July 18, 2017. (View)
- Management of Penicillin and Beta-Lactam Allergy. Antimicrobial Treatment Guidelines for Common Infections. The New Brunswick Provincial Health Authorities Anti-infective Stewardship Committee. Drugs and Therapeutics Committee. Optimal antimicrobial care for our patients and our future. 25-34. February 2016. http://bit.ly/NB-Penicillin-allergy-assessment-pg25
- Figure 1: Management Diagram: pg 26: http://bit.ly/NB-Penicillin-allergy-management-diagram-pg26
- Figure 2: Matrix of Beta-Lactam Cross Allergy: pg 27: http://bit.ly/cross-matrix-beta-lactam-allergy-pg27
- Beta-lactam Allergy Handout http://bit.ly/TCMPBLAa. Provided with permission of Dr. Cesilia Nishi, Pharm D. Adapted from Antimicrobial Treatment Guidelines for Common Infections. The NB Provincial Health Authorities Anti-infective Stewardship Committee. Drugs and Therapeutics Committee. Optimal antimicrobial care for our patients and our future. June 2016.
References
- Pena, AP et al. Relationship between quinoloneuse and emergence of ciprofloxacin-resistant escherichia coli in bloodstream infections. Antimicrobial Agents and Chemotherapy. 39(2):520-4. 1995. (View) doi: 10.1128/AAC.39.2.520
- Solensky R, Khan D, Bernstein I, et al. Drug allergy: An updated practice parameter. Allergy. Asthma. Immunol. 2010;105:259-273.e78. (View with CPSBC or UBC) doi:10.1016/j.anai.2010.08.002
- Pichichero ME. A review of evidence supporting the American Academy of Pediatrics recommendation for prescribing cephalosporin antibiotics for penicillin-allergic patients. 2005;115:1048-1057. (View with CPSBC or UBC) doi:10.1542/peds.2004-1276
- Gonzalez-Estrada A, Radojicic C. Penicillin allergy: A practical guide for clinicians. Clin. J. Med. 2015;82:295-300. (View) doi:10.3949/ccjm.82a.14111
- Lagacé-Wiens P, Rubinstein E. Adverse reactions to β-lactam antimicrobials. Opin. Drug. Saf. 2012;11:381-399. (Request with CPSBC or view UBC) doi:10.1517/14740338.2012.643866

Very good comments. As the author mentioned many of these reactions are viral exanthema or even an amoxil rash with Mono.
However referral to an allergist for most patients is not feasible or cost effective. Lab testing is also costly.
Great article
Great summary of the issue and a rational approach.
Thanks for clarifying this rational approach. Many allergists (apparently) also provide a test dose under medical supervision to clinincally rule out reactivity (as per https://www.uptodate.com/contents/significance-of-negative-penicillin-allergy-skin-testing-beyond-the-basics).
Observe that penicillin allergy is less apparent in the elderly
Thank you for addressing this important topic. I am wondering if you can comment on an approach to Type IV/maculopapular rashes following amoxicillin in children as this is so common. While skin tests may not be appropriate for all affected, it also doesn’t necessarily seem appropriate to write off beta-lactams for life for all the reasons addressed in your article. Could you please provide some child-specific recommendations, thank you!
Most “penicillin allergies” are likely viral exanthems of childhood. Do we skin test all of them?
Hi,
Sorry, I am really slow on responding. I also don’t know how to log on as author, but for mild reactions in childhood (assuming the patient is now an adult) I offer to give a test-dose under medical supervision and by-pass the skin testing step as the likelihood of anaphylactic reaction is very low. I do discuss the risk/benefit with patients including the very small likelihood of a more severe reaction but reassure the patient that we will observe and treat them in the case of reaction to the test dose. This process also addresses the lack of resources for skin testing.
Of interest, several places have created a “skin testing team” staffed by nurses or pharmacists trained to read the skin reaction, making skin testing easier to access and more timely for inpatients who need immediate antibiotic therapy. See these links:
https://www.ncbi.nlm.nih.gov/pubmed/28575226
https://sunnybrook.ca/media/item.asp?c=1&i=1613&page=524&f=bedside-penicillin-allergy-testing
Hope that helps