Author
Omesh Syal, MD, CCFP (biography and disclosures)
Disclosures: Dr. Omesh Syal is the Chair of Divisions of Family Practice – Prince George, and Chair at HDC. Mitigating potential bias: Recommendations are consistent with published guidelines and current practice patterns.
Disclaimer: The Health Data Coalition (HDC) is a physician-led data-sharing initiative that encourages reflection and collaboration with colleagues and facilitates quality improvement in patient care through its HDC Discover application. HDC is a not-for-profit organization, funded by the Family Practice Services Committee (FPSC) and powered by the enthusiasm and dedication of a growing network of family physicians from across the province, with the primary focus of empowering physicians and clinics to understand and use their data for practice improvement.
What I did before
Type 2 diabetes is the most common form of diabetes (90% of all cases), with some people at higher risk of developing type 2 diabetes, including those who are living with excess weight and those who come from historically marginalized groups.1
Although type 2 diabetes typically occurs in adults, rates among children are rising. According to BC Ministry of Health data, the number of people diagnosed with type 1 or 2 diabetes in Prince George annually is 544. This population group often becomes complex in nature, with associated comorbidities to manage.
I was identifying diabetes in more of my patients and was curious to see if my hunch of the increasing prevalence was reflected in my patient panel. Prior to registering with the Health Data Coalition (HDC) and having access to a tool like HDC Discover, I would call my Practice Support Program (PSP) coach, and set a time to meet, which may result in a Quality Improvement Facilitation Cycle. We would choose a topic and run practice analysis and reports within our Electronic Medical Records (EMR). From here, we would be able to tailor the clinical quality improvement question. It was more time-consuming than using the HDC Discover application.
What changed my practice
The HDC Discover application, which is currently in use by primary care physicians across British Columbia, provides secure access to aggregated clinical measures while maintaining both patient and physician confidentiality. It is a service that was envisioned by innovative physicians, backed by the Divisions of Family Practice, who believe in the collective impact concept. I am the Board Chair of the Prince George Division of Family Practice and the Chair of the HDC for which I am humbled to carry forward the insightful work by my mentors and peers before me.
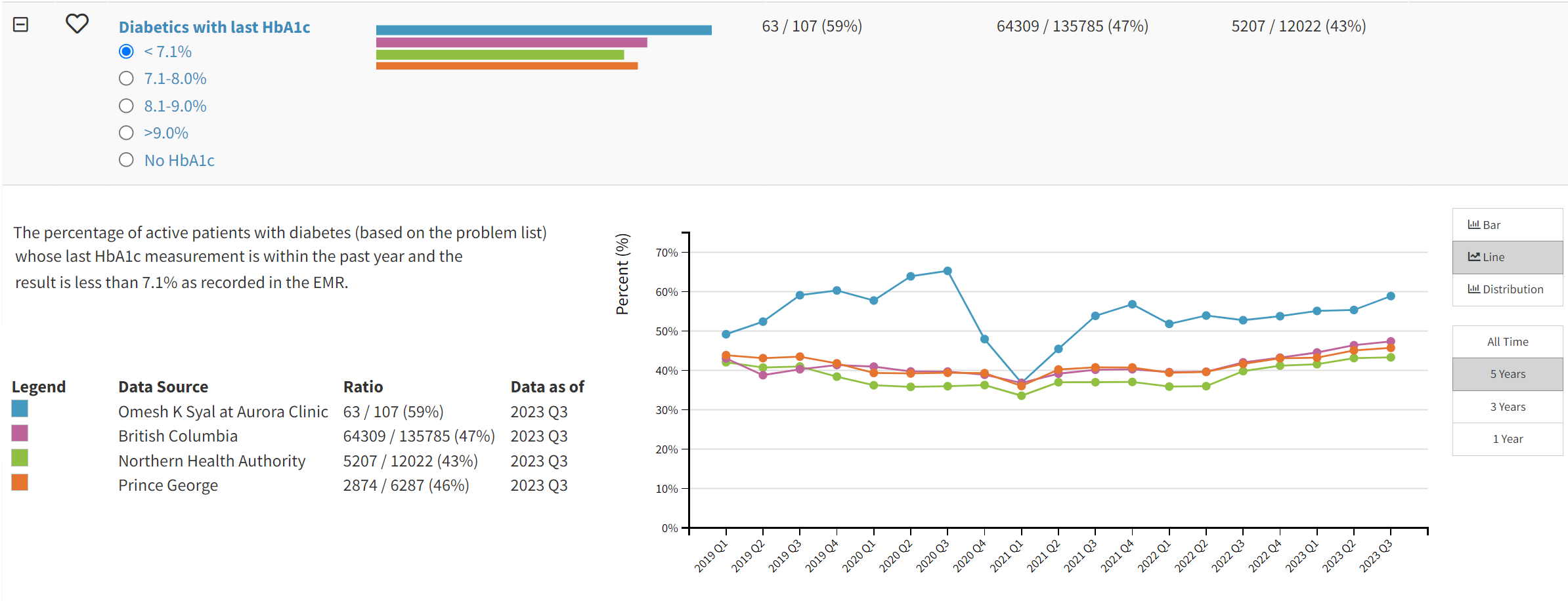
HDC Discover allows me to easily visualize my data and provides a view outside of my own clinic through aggregates of my peers within my geographic region and province. While reviewing my HDC data, I noticed that the average HbA1c for my patients living with diabetes was higher than what I thought it should be. I also noticed that this was true in the larger community in which I practice.
Figure 1. Dr. Syal’s patients living with diabetes with HbA1c less than 7%
After looking deeper into EMR data for patients with HbA1c over 7%, I observed that the patients who had the most challenges with their blood sugar were also the patients who needed complex care with other comorbidities such as coronary artery disease, COPD, and renal failure. Complex patients often require more time and attention to develop a care plan that is revisited and updated as needed.
Normally I take Friday afternoons to catch up on my practice, so I promptly worked within my EMR to identify a patient list and delegated to my staff to use Friday afternoons to call in our patients living with complex diabetes for a longer consultation on their medications, diet, and exercise. Taking the time to review my patients and ensure I had a plan in place, helped me feel in better control of my practice. This process allowed me to find joy in my work again. It validated myself as a physician, providing great primary care.
It’s difficult to find time to test a different process to benefit both patient outcomes and practice objectives. Each physician will find what works best for them, but I want to emphasize that the results of the work are worth it. Patients expressed their happiness that I was spending time with them, and over time, many better understood which individual data points I routinely check and empowered their own self-management plans. I feel a sense of accomplishment that my most complex patients take their disease management seriously.
What I do now
I now book 20 minutes at the end of every quarter to look at my favourite HDC Discover measures to keep an eye on key practice data points, like HbA1c trends and other patient groups that would benefit from the additional support. I can see when change is sustained or if I may need to call in my PSP coach to look at something more closely with me. Identification and familiarity of my patients with complex care needs is essential for the overall management of my practice, which is why my staff also keeps tabs on these patients and recalls back in for visits if needed.
I have found it extremely rewarding to spend time with my patients with complex care needs and provide this level of care. My patients also know what to expect, as they know patients check their HbA1c every 3 months as appropriate, regularly review their medication list, and return to clinic for an annual (longer) complex care visit. After completing complex care visits for these patients, we directly saw the reduction in A1c demonstrated so clearly on my graphs in HDC Discover.
When I first started focused patient management for my patients with blood sugar challenges and additional complexities, it was initiated and coordinated between myself and my MOA, but things are changing, and I am not alone. Going forward, I plan to include a community clinical pharmacist to support my patients with complex care needs and I can still rely on my EMR and HDC Discover as monitoring tools. Near the end of the quality improvement project, I realized how many of my patients have complex care needs and the need to incorporate more community resources that I can incrementally build into my practice (i.e., physical therapy, community nursing).
In my case, the investment of an afternoon helped me utilize my clinical time in a way that benefits both patient outcomes and practice objectives. Use of the FPSC chronic disease management or complex care incentive fee service codes or the Longitudinal Family Practice payment model improves patient care by making sure we are spending time not only with the patient but on their chart as well. It allows for an accurate updated patient chart that can be shared with other providers or health facilities, which improves communication, as well as respecting patient choices.
I highly recommend registering with the Health Data Coalition and becoming more familiar with your measures within the HDC Discover application to recognize your contribution. We, as a collective profession, can make a positive impact on our own practices and larger communities.
Resource
Physicians interested in learning more about the Health Data Coalition and utilizing HDC Discover can reach out to info@hdcbc.ca or visit https://hdcbc.ca.
Reference
Provincial Health Services Authority. BC Community Health Profile, Prince George. Prince George: Provincial Health Services Authority, 2021. Page 15. Accessed April 10, 2024. (View PDF)

I applaud the physician for improving their sense of well-being. I regret that the plurality of the article, however, did not offer more information about the patient’s and their outcomes.
Does HDC work for Ontario?
In terms of applying an epidemiological approach to the medical practice, this is a good thing. However, the way about getting to the data is really very short sighted and it is so because of ideological reasons, in this case everything is better than a governmental take on the issue (since is more cost effective and little to no associated fees; albeit in the case of HDC it looks like being funded by the government via the Master Agreement with the Doctors of BC). This despite having PharmaNet the crown jewel of information systems in health care in Canada.
PILS (the Provincial Informational Laboratory System) in BC, a designated databank and collected by PHSA (which just sits on that information) and passed it on the MoH, which also sits on that information with the excuse that the database is to complex to be used, could very well provide all epidemiological information a clinical practice might need on the subject brought by the article and many more.
Heck, by putting together medication information (PharmaNet) with clinical lab results (PILS), one can even see what drugs work the best. But it looks almost that it is destined that the two shall never meet, kind of pre-ordained…
I admire your work and continued dedication!