Authors
- Dr. Ken Tan (biography, no disclosures)
- Dr. Julia Stewart (biography, no disclosures)
- Dr. Doug McTaggart (biography, no disclosures)
- Dr. Sandra Lee (biography, no disclosures)
- Chase Simms MPH (biography, no disclosures)
What I did before
Historically, when a patient presented with acute diarrhea and I suspected an infectious etiology, my patient would need to collect multiple stool samples – for C&S, C. difficile, and sometimes even an O&P (or two). This could involve sequential testing (and possibly repeat office visits), with several drop-offs at the lab for the stool samples. Ultimately it equated to hassle for patients and inefficiencies for all!
What changed my practice
A new laboratory test has been introduced in BC: the Infectious Diarrhea Panel (IDP). This combines the previous three tests with a single-specimen test, and replaces the stool C&S and O&P in BC. Note, however, that standalone C. difficile tests are still available. The IDP incorporates nucleic-acid amplification test with other methods, including antimicrobial susceptibilities where applicable, and is more sensitive and provides results quicker than the traditional tests. It detects the 14 most common and relevant pathogens that cause infectious diarrhea (see Figure 1), some of which (e.g., norovirus and Shiga toxin-producing E. coli [STEC]) were not previously routinely detectable. Previously it would have been difficult to roll out the IDP across the province, but due to the rapid implementation of COVID-19 testing infrastructure, it is now feasible.
A companion document, Infectious Diarrhea – Guideline for Investigation, was developed to inform the best appropriate use for the IDP, and how to interpret its results. This guideline applies to a broad population with suspected community-onset infectious diarrhea, including C. difficile infection (CDI). The document includes a simple approach for the diagnostic workup of suspected infectious diarrhea, including repeat testing (if needed). As well as summarizing the clinical presentation and management of each pathogen, this BC guideline is the foundational document that BC laboratories will reference for the indication and use of the IDP.
Figure 1. Pathogens that are included in every laboratory’s Infectious Diarrhea Panel (IDP)a
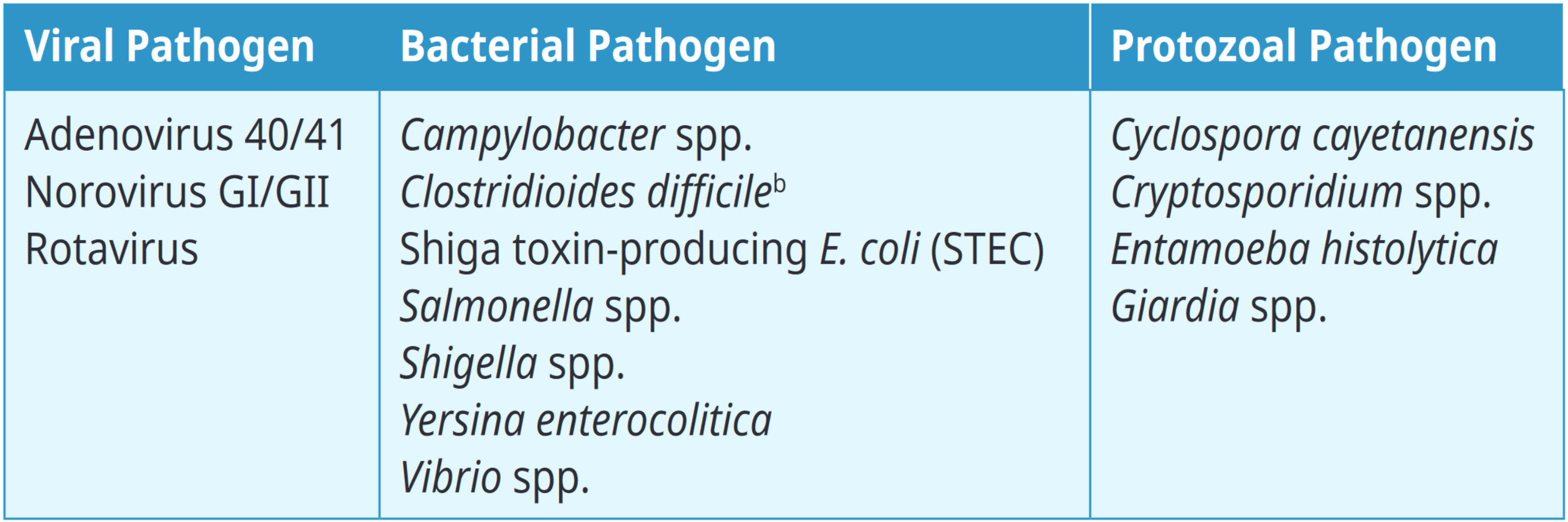
a. The list of pathogens may be modified periodically, in line with changes in epidemiology and technology
b. C. difficile is not routinely reported in those under 2 years old
What I do now
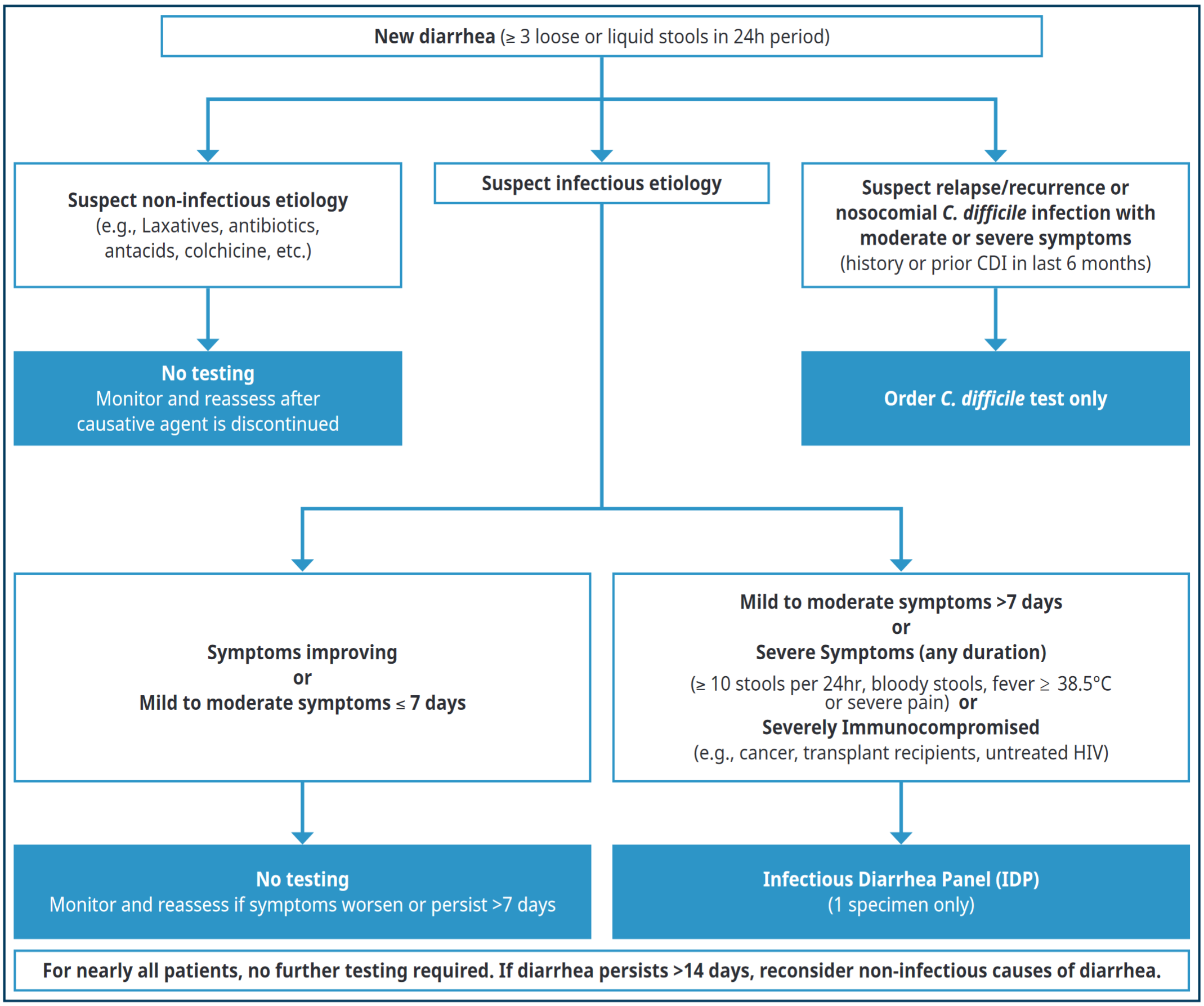
Considering most acute diarrhea self resolve, and in support of diagnostic stewardship, I have become more conscious about ordering tests only when they are necessary and appropriate. If an immuno-competent patient presents with acute, mild to moderate diarrhea of ≤ 7 days (or their diarrhea is clearly resolving) and I suspect an infectious etiology, then I generally have them monitor their symptoms and do not order any tests.
Who do I send immediately for a stool IDP? Any patient who is severely immuno-compromised, anyone whose mild-moderate diarrhea persists beyond 7 days and is not clearly resolving, and anyone with signs of severe diarrhea (regardless of duration), i.e., > 10 stools per 24 hours, bloody stools, fever ≥ 38.5, or abdominal pain. I also send for testing anyone whose mild-moderate diarrhea persists beyond 7 days and is not clearly resolving.
When I give my patient a requisition for the IDP, I explain that this is a new, “high tech” stool test that replaces the older stool tests, only needs one specimen, and is more precise. I let them know that we will receive the results quicker, and they will not need to repeat the test, nor provide multiple stool samples.
What about stool C. difficile tests? I can continue to order them – and they are useful when I suspect a relapse or recurrence of C. difficile in a patient with a C. difficile colitis history. Rather than requesting an IDP test (which costs $105), it makes sense to send my patient off with a requisition for a one-time C. difficile stool test when my clinical suspicion is very high. C. difficile test costs $16 to $49. I also order a standalone C. difficile stool test in a patient who has been hospitalized for more than 5 days and who develops acute nosocomial diarrhea.
Do I repeat the IDP? No – I request only one IDP test per diarrheal illness.
Figure 2 outlines the diagnostic algorithm I utilize for the workup of acute diarrhea. I also reference the BC guideline: Infectious Diarrhea – Guideline for Investigation, which provides more detailed discussion and includes information on patients who have swum in or consumed contaminated water.
Figure 2. Diagnostic workup of acute diarrhea
Guidelines and Protocols Advisory Committee (GPAC). Infectious Diarrhea – Guideline for Investigation, 2022. Available from: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-resources/bc-guidelines/infectious-diarrhea-guideline-for-investigation
Management and Treatment
For most patients with infectious diarrhea, treatment is supportive. If the IDP is positive but my patient is healthy and no longer symptomatic, then generally antimicrobial treatment is not indicated. The rationale behind this lies in the very high sensitivity of the IDP, meaning that this test may detect very low amounts of pathogens, non-viable pathogens (i.e., resolving infections), or cases of asymptomatic infection/colonization.
Targeted antimicrobial management is guided by my patient’s clinical history, course of illness, and the pathogens identified by IDP. There are certain situations when antimicrobial therapy is absolutely required, such as when the IDP is positive for Entamoeba histolytica or typhoidal Salmonella, and in patients with moderate to severe illness who are positive for Vibrio cholera. Antimicrobial treatment may also be warranted in patients who are at risk of transmitting certain pathogens to others (e.g., Giardia spp. and Shigella spp.). Table 1 below (Summary of clinical presentation and indications for antimicrobial treatment) is very helpful, and if I have more questions, I refer back to the Infectious Diarrhea – Guideline for Investigation as it provides further nuanced discussion around the diagnosis and management of infectious diarrhea.
As previously, a positive C. difficile result does not differentiate between infection and asymptomatic colonization, for both IDP and standalone C. difficile stool tests. I only treat positive C. difficile tests in patients who are symptomatic and where C. difficile is the likely cause.
If the IDP detects positive STEC (Shiga Toxin-producing E.coli), then the recommendation is to stop and/or avoid any antibiotics, due to risk of hemolytic uremic syndrome (HUS). Patients with high-risk strains (e.g., E.coli O157:H7) require immediate assessment and may require hospitalization.
Even if a pathogen is identified where only supportive measures are available (e.g., Norovirus), my patient and I receive a diagnosis that allows me to provide a prognosis and give advice around transmissibility to others and strategies for avoidance in the future.
Occasionally I may need to reach out to the specialists to inquire about atypical clinical scenarios. If I have a straightforward question about what tests to order for a specific pathogen or environmental exposure, I may contact my local medical microbiologist for advice. However, for patients with more complicated clinical histories and/or who are severely immunocompromised, I would consider referral to an infectious diseases specialist.
The combination of the new Infectious Diarrhea Panel (IDP) test and the Infectious Diarrhea – Guideline for Investigation have indeed upped my game in the diagnosis and management of acute infectious diarrhea, and is a clear win-win for me and my patients!
Table 1. Summary of clinical presentation and indications for antimicrobial treatment (download)
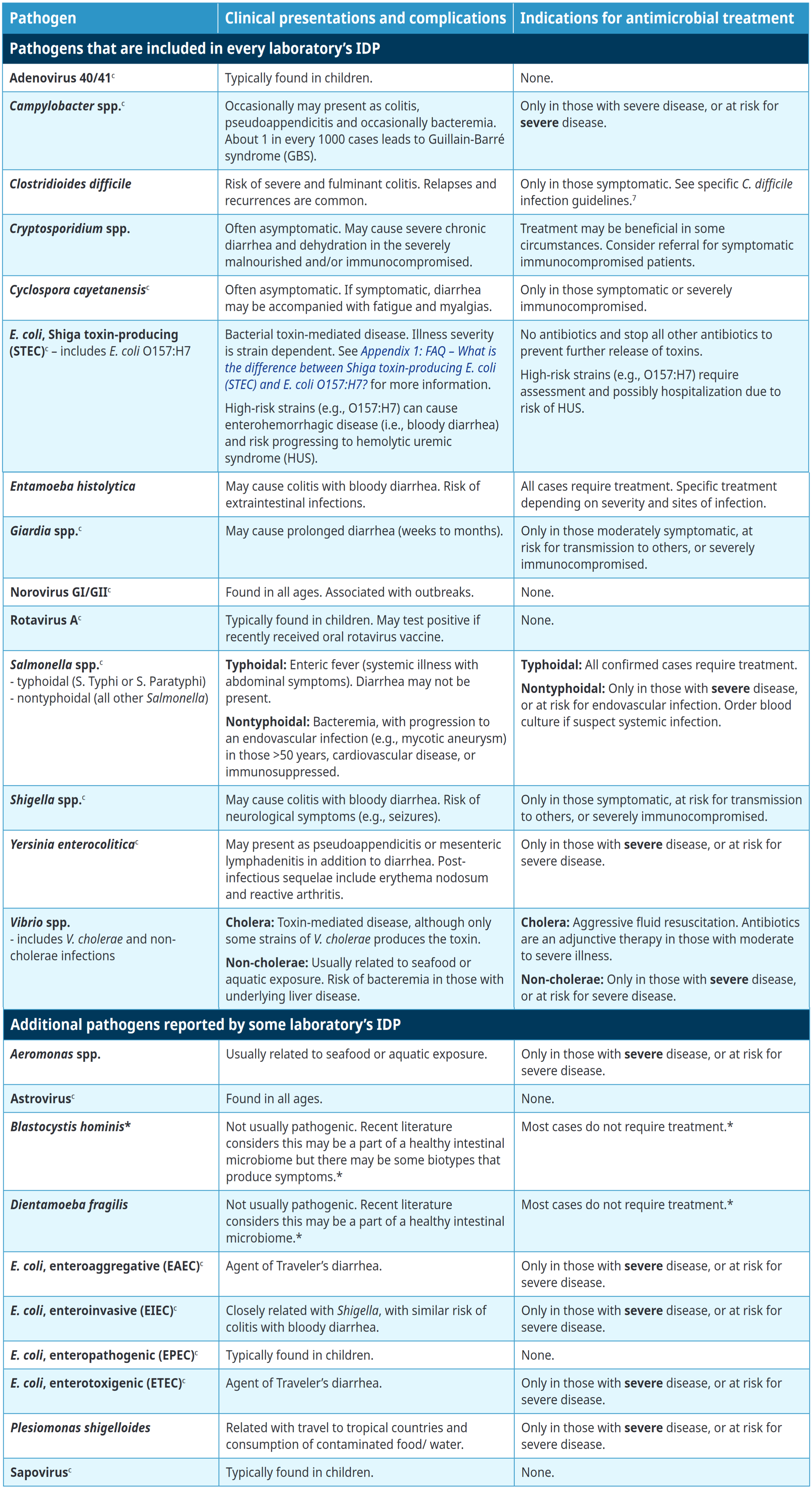
c. These pathogens are reported to public health
* Refer to Appendix 1: FAQ – What about Blastocystis hominis and Dientamoeba fragilis? for more information.
Handout for patients
Appendix 3: Patient instructions – Collection of fecal swab. Accessed August 22, 2023. View
Reference
Guidelines and Protocols Advisory Committee (GPAC). Infectious Diarrhea – Guideline for Investigation. Guidelines and Protocols Advisory Committee (GPAC); 2022. Accessed August 22, 2023. (View)

Fantastic test that I have found very useful clincally already.
One test that is NOT included in this IDP and we should be ordering more often: Strongyloides serology. It is present in 40% of foreign-born Canadians. That’s 2.5 million Canadians.
So I always try to order this if someone has vague GI symptoms / is at risk (i.e. they walked barefoot in Africa, Asia and Central or South America)
Source: https://www.cmaj.ca/content/194/3/e89
Very useful.
I wonder about suspected food poisoning from restaurants, community dinners, etc. Where does this test fit in?
I recall some food poisoning causes vomiting quickly (staph?) — this test would not help, but quite a lot is diarrhea illness. This has legal & public health implications.
Years ago at our clinic party for a departing staff they all went down with salmonella. The source was easy to track – raw cheesecake made on the premises. (No doctors were ill because we all left before dessert for a meeting at our office.)
Anyone knows if this is available in other provinces?