Authors
Karin Kausky, MD CCFP FCFP Dip. Sport Med. (biography and disclosures), Tracy Monk, MD (biography and disclosures), and Daniela Michel, MPH (biography, no disclosures)
Disclosures: Drs. Karin Kausky and Tracy Monk: Members of the PathwaysBC Provincial Resource Committee. PathwaysBC is a collaborative non-profit GPSC-initiated project, freely available to all BC physicians and their teams. Received payments for being on the resource committee on PathwaysBC. Mitigating potential bias: Recommendations are consistent with current practice patterns and published guidelines. Only published trial data is presented.
What I did before
Antimicrobial resistance is recognized as a top public health threat and is estimated to be directly responsible for 5,400 deaths and $1.4 billion in health care costs in Canada in 20181 which underlines the critical importance of wise prescribing of antibiotics.
While antibiotic resistance can occur naturally, the most important driver of antibiotic resistance is inappropriate or unnecessary prescribing.2, 3 Additionally, shorter durations of treatment are recommended for many indications, and extended courses that continue beyond resolution of the infection predictably increase the risk of antibiotic resistance.4 The misuse and overuse of antibiotics accelerate antibiotic resistance. It is of vital importance to prescribe antibiotics only when needed and according to current guidelines. Staying up to date on prescribing guidelines can be a challenging task, and all too often the tried and true prescribing habits from years before take precedence over seeking the latest evidence.
In the past, looking up the most appropriate antibiotic involved rummaging through my desk for an outdated hard copy of Bugs & Drugs, or just prescribing in my usual patterns.
What changed my practice
A resource to support good antibiotic stewardship is Bugs & Drugs, a continuously updated, local, and evidence-based prescribing guideline. Bugs & Drugs is a comprehensive guide to antimicrobial therapy and an aid to wiser antibiotic use in front-line practice. The guide is available as a website and for offline use as an app (iOS and Android) and is free of charge for all BC prescribers. Bugs & Drugs contains evidence-based, peer-reviewed, and antibiogram-directed guidelines and treatment recommendations. It is continuously updated with the latest guidelines and recommendations.
Figure 1: Bugs and Drugs 2.0 App
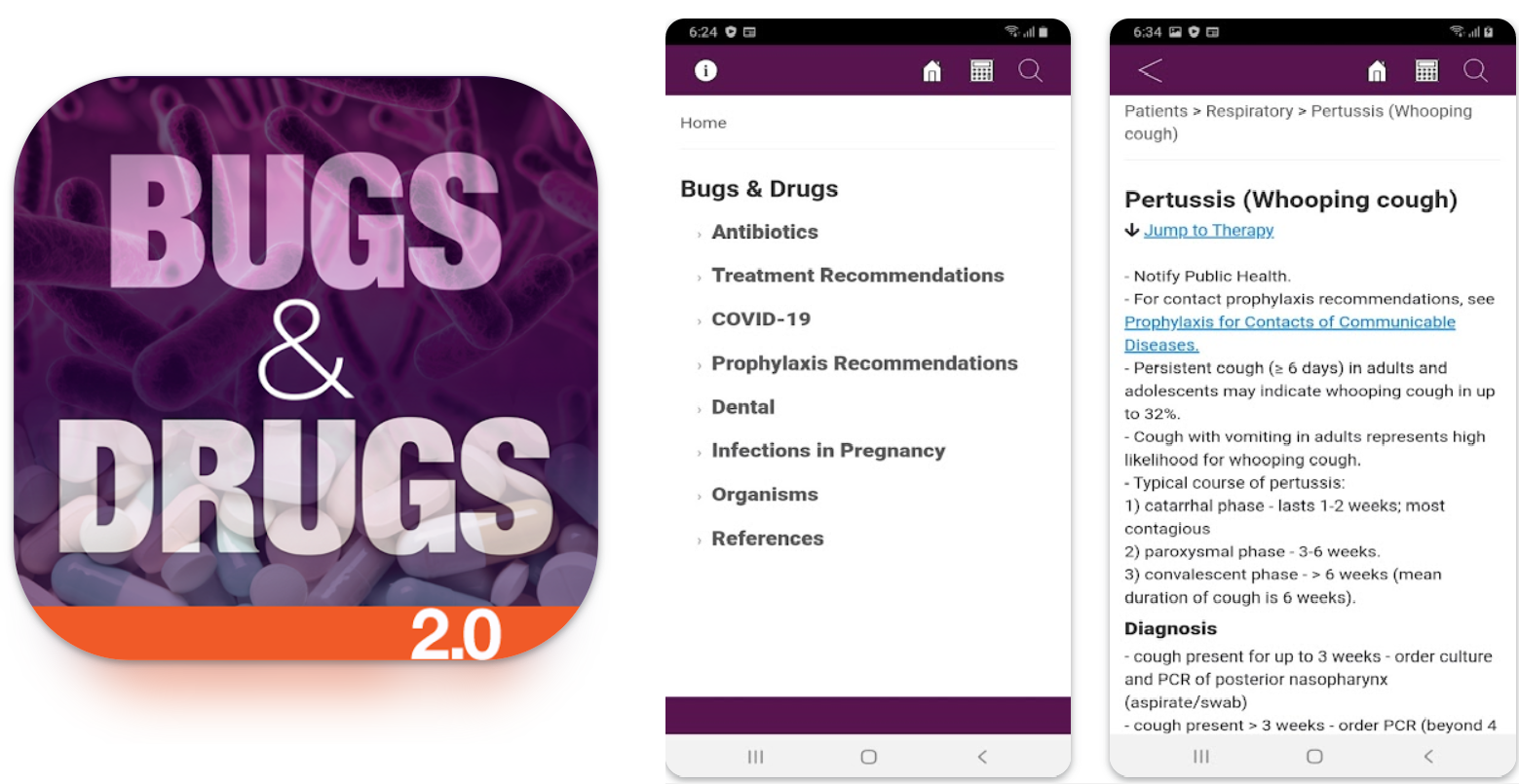
The guide offers information on over 70 antimicrobials (e.g., spectrum of activity and/or dosing recommendations), empiric management advice (for adult and pediatric, fungal, parasitic, ophthalmic) for more than 140 clinical syndromes, a culture-directed section for over 90 infections and clinical significance and empirical management of 172 potential pathogens.
Having free access to this up-to-date resource allows for appropriate antibiotic practices to be the accepted norm in clinics and practices. Antimicrobial therapy guidelines improve adherence with standards of care and are a core practice of good antimicrobial stewardship.
Users of the Pathways BC website (https://pathwaysbc.ca/info) can also access quick links to Bugs & Drugs treatment recommendations for common infections. For community-based infections, it is faster to get to the right page of Bugs & Drugs by typing the name of the infection in the Pathways search bar.
Pathways also contains Bugs & Drugs information for patients that can be emailed to patients directly from the secure PathwaysBC.ca website during an office visit.
What I do now
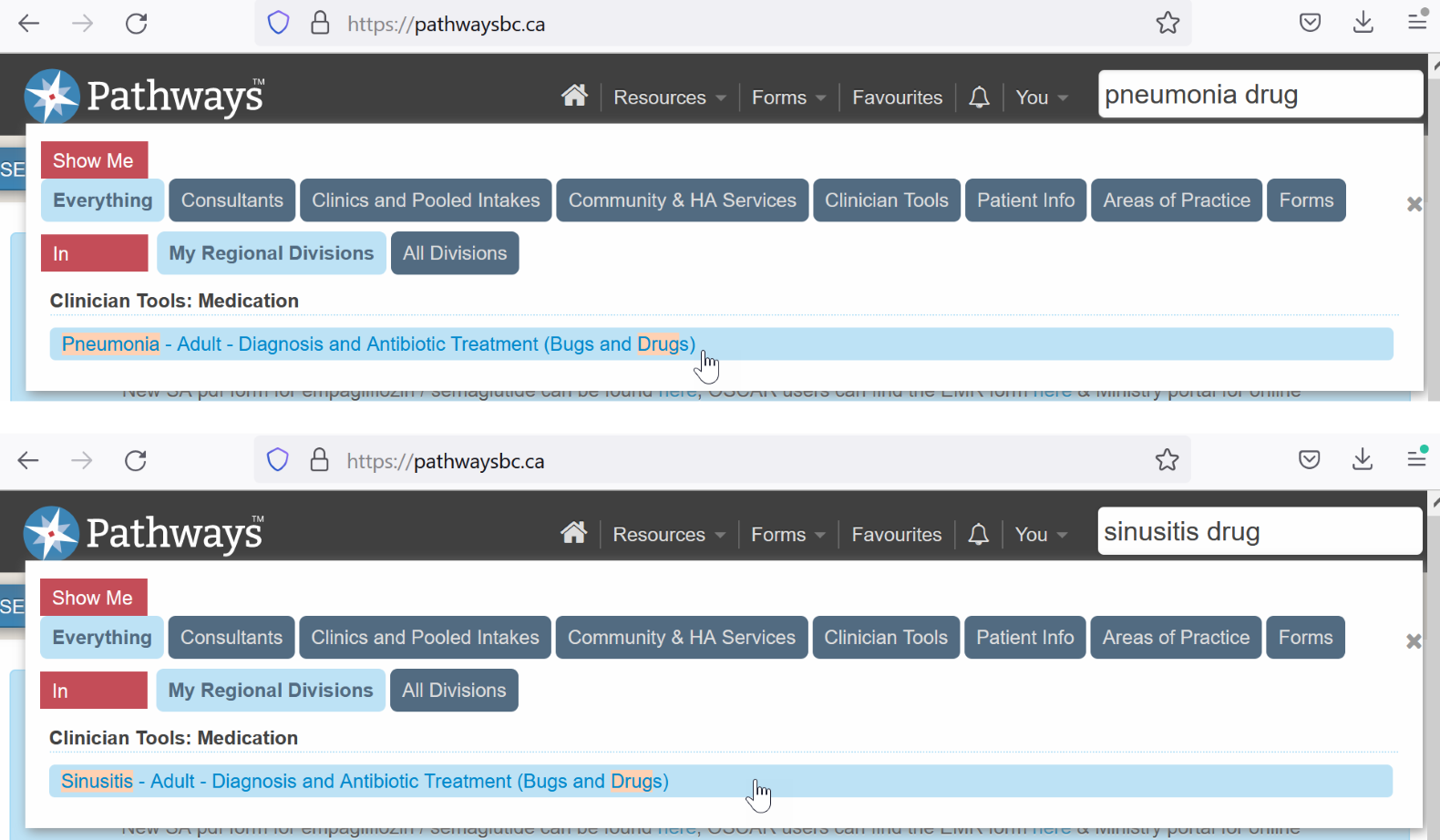
Every time I prescribe an antibiotic now, I check the Bugs & Drugs guideline and am often surprised by the short durations of treatment recommended. As a daily Pathways user in BC, I type the name of the infection in the Pathways search to get quickly to the right page of the Bugs & Drugs manual. E.g., try typing PNEUMONIA or SINUSITIS or BITE or CELLULITIS in the Pathways search bar (click here for a quick PDF overview).
When we use Pathways to search the infection we are treating, Choosing Wisely recommendations often show up as well. If I only want to see the antibiotic drug recommendations in the Pathways search we add the word DRUG after the name of the infection e.g., PNEUMONIA DRUG.
Figure 2: Examples from PathwaysBC.ca
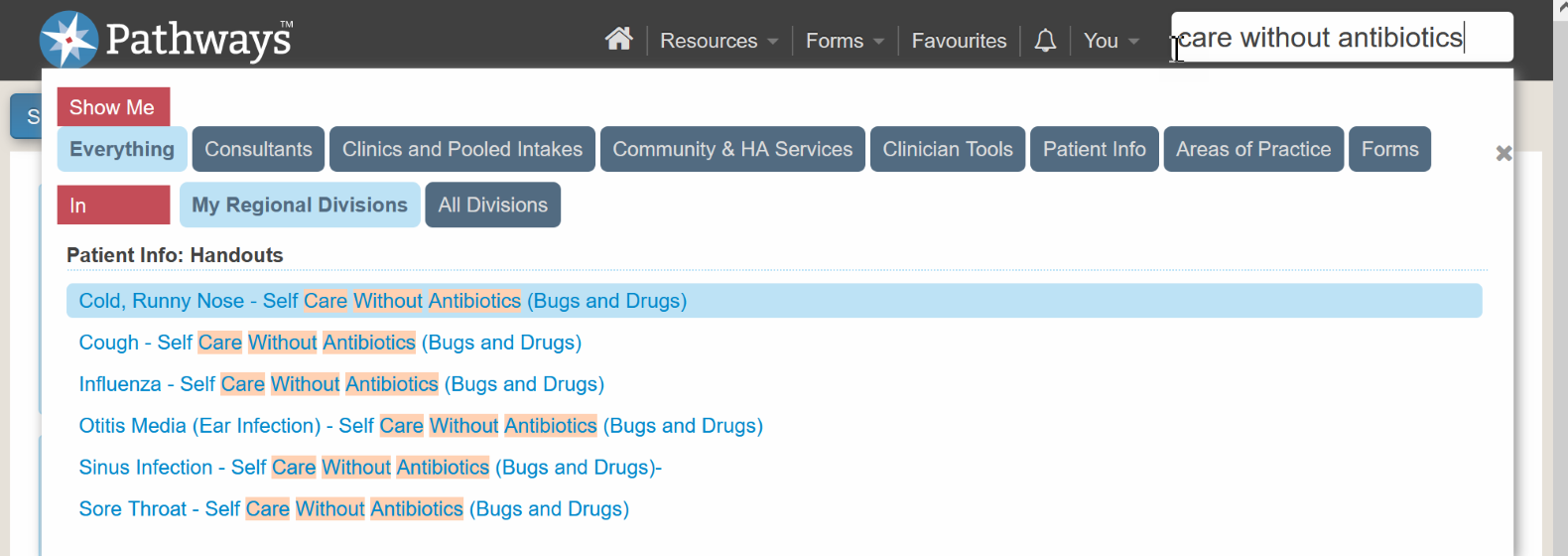
Often patients ask for an antibiotic but do not need one for their viral illness, and it is helpful to use the email-able Bugs & Drugs patient info items about self care for cough or runny nose or sore throat without antibiotics. To see the email-able patient info, try typing CARE WITHOUT ANTIBIOTICS in the Pathways search.
Figure 3: Example from PathwaysBC.ca
In some cases, a specific antibiotic may not be an optimal first choice e.g., ciprofloxacin and other fluoroquinolones. Sometimes patients with UTIs make a specific request for ciprofloxacin and it is helpful to be able to use the Pathways search to quickly access recommendations about avoiding fluoroquinolones from the BC Provincial Antimicrobial Clinical Expert Group (PACE) by typing CIPROFLOXACIN in the Pathways search.
Optimizing the use of antibiotics in everyday practice is a critical component to effectively treat infections while protecting patients from harm caused by unwise prescribing and to combat antibiotic resistance. Having a quick reference tool at our fingertips has changed our approach to antibiotic prescribing. We now have the ability to quickly look up recommendations during the visit. The reference also allows for a deep dive into the recommendations when time permits and has strengthened our understanding of wise prescribing.
Resources
- Bugs & Drugs: https://www.bugsanddrugs.org
- Bugs & Drugs app:
- Pathways: https://pathwaysbc.ca
- Monk T, Graham N, Kausky K, Thomasse M, Gallagher R. Practice tip (for BC practitioners) utilizing PathwaysBC beyond specialist lookups — finding patient handouts, requisitions, point-of-care tools. This Changed My Practice, UBC CPD. https://thischangedmypractice.com/practice-tip-for-bc-practitioners-utilizing-pathwaysbc. Published March 22, 2022. Accessed January 10, 2023.
References
- Council of Canadian Academies. When antibiotics fail. The Expert Panel on the Potential Socio-Economic Impacts of Antimicrobial Resistance in Canada. Ottawa, Canada: Council of Canadian Academies; 2019. https://cca-reports.ca/reports/the-potential-socio-economic-impacts-of-antimicrobial-resistance-in-canada. Accessed January 10, 2023.
- Chatterjee A, Modarai M, Naylor NR, et al. Quantifying drivers of antibiotic resistance in humans: a systematic review. Lancet Infect Dis. 2018;18(12):e368-e378. doi:10.1016/S1473-3099(18)30296-2 (View with CPSBC or UBC)
- Holmes AH, Moore LS, Sundsfjord A, et al. Understanding the mechanisms and drivers of antimicrobial resistance. Lancet. 2016;387(10014):176-187. doi:10.1016/S0140-6736(15)00473-0 (View with CPSBC or UBC)
- Grant J, Saux NL; members of the Antimicrobial Stewardship and Resistance Committee (ASRC) of the Association of Medical Microbiology and Infectious Disease (AMMI) Canada. Practice Point: Duration of antibiotic therapy for common infections. J Assoc Med Microbiol Infect Dis Can. 2021;6(3):181-197. Published September 30, 2021. doi:10.3138/jammi-2021-04-29 (View)

I love my Bugs and Drugs app! I use it nearly every day I practice.
Great suggestion
I tried downloading Bugs and Drugs on my phone and they want a credit card.
Excellent review of the relevant tools to minimize the big problem of drug resistance and other antibiotic serious side effects
Excellent resource . I also use prescribing wisely as well as Uptodate
This was a great article. I am fairly new to BC as a family doctor and this absolutely inspired me to learn more about using Pathways in general. I do a lot og Urgent Care as well as longitudinal care and this will help reduce antibiotic prescribing overall I think.
Hi. I would just also encourage the authors to consider the first line app. It has the advantage of local data derived from local antibiogram resistance data and also includes specific populations such as pregnant persons, gyne and pediatrics.
Great resource. Thanks for alerting us to this growing issue of drug resistance.
I know this is an excellent app, and that drug resistance is a huge problem.
As a Pediatrician, I treat young adults up to 20 years old.
For uncomplicated urinary tract infections in particular, I use Fosfomycin Tromethamine. In practice, it is not easy for patients to access a lab and then wait for results. In Vancouver, for example, sometimes the only alternative is to go to BC Children’s Hospital Emergency Room – which is the worst use of the ER. For patients who are prone to uncomplicated urinary tract infections, and know exactly when they have an infection, I make sure they have a supply of Fosfomycin at home.
I would be very interested to hear what other physicians do.
The Community Antimicrobial Stewardship program at the BC Centre for Disease Control facilitates access to Bugs and Drugs in BC. If you have any questions about the resource or difficulties in accessing it, please feel free to reach out to info@antibioticwise.ca for assistance. We’re happy to hear that so many find Bugs and Drugs (and Pathways) so useful in their practice.
I use Bugs and Drugs app daily. It is such a useful and practical guide for prescribing antibiotics.
I use pathways fairly regularly, but did not think about its use for this. Firstline as mentioned is like a further extension of Bugs and Drugs and free from FHA. It is site specific for management of resistance and sensitivities.
I agree with this and use the app
When the bug is reported I often check Firstline from Providence Health to select the most appropriate antibiotic.