Dr. Steve Wong (biography and disclosures)
Editor’s note: The use of smartphones and mobile, handheld computing devices like the iPhone, iPod Touch and others among physicians is remarkable. In 2011, 81% of US physicians own a mobile device1, 54% of physicians access medical information on their smartphone during patient visits2. Currently, the most popular devices are Apple iOS devices (32% iPhone/iPod Touch, 22% Blackberry, 16% Palm, 9% Windows, 4% Android, 2% Symbian1).
In response to reader requests and the increasing interest in mobile apps, we are launching a series of articles highlighting useful iPhone apps. These will appear approximately once every three months.
If you have app suggestions, or if you use an Android device and would like to submit an article, please email us at feedback@thischangedmypractice.com.
We hope you enjoy this series of articles.
What I did before
A large part of my practice is focused on the management of diabetes. A key recommendation from the CDA guidelines is the achievement of A1C targets of 7%. Also, when appropriate, I encourage patients to perform self-monitoring of blood glucose levels. I try and teach all my patients what the role of the A1C is as well as how to use their home measurements to guide treatment.
More often than not, patients either don’t test at home at all, or if they do, they test only in the fasting state in the morning, which may give falsely reassuring results as they assume the rest of the day looks similar.
In followup visits, when patients are reviewing their lab results, I often found that patients assumed the A1C is a numeric average of their own glucometer readings (eg. “My A1C is 7.2 – my average glucose must be around 7”). I advise them that the A1C has a nonlinear correlation with average glucose readings over the last 3 months. In fact, when I point out to them that an A1C of 7.0% (eg. “at target”) represents an average glucose level of 8.6 mmol/L, many patients respond with surprise and say “wow, that’s actually pretty high.”
These kinds of discussions have been useful in encouraging adherence to therapy and improved understanding of disease pathophysiology, however, I often found myself guesstimating values, which obviously introduces a potential for misleading advice.
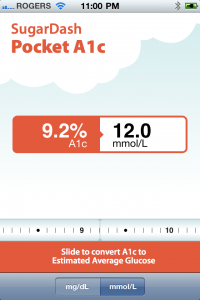
A free app called Pocket A1C makes it extremely easy to illustrate to patients the relationship between their A1C and average glucose readings. They can immediately see that I’m not simply making up a number, but more importantly, the real-time, animated sliderule really seems to impact patients when they see me scrolling up and up to get to an A1C of 9.2 as well as see their average glucose of 12 mmol/L.
Get Pocket A1C here (free):
http://itunes.apple.com/ca/app/pocket-a1c/id317041063?mt=8&ign-mpt=uo%3D4
What I do now
I now use Pocket A1C several times a day. This direct illustration from a lab value (A1C) to a number they may be intimately familiar with (their own glucometer readings) greatly increased patient acceptance of recommendations for intensification of treatment. I also found the app saved me time in explaining the utility of the A1C assay.
Pocket A1C has helped me achieve targets in patients who may have been reticent to accept more intense treatment and I believe helped me educate my patients more effectively about their diabetes.
References:
1. Manhattan Research
2. SDI’s Mobile and Social Media Study, 2010

Such an easy tool for me and for my patients! I believe it will lead to encouraging better compliance with regular testing and consistent dietary moderation!
A very useful app. patients are often confused between the A1C and the glucometer readings as the numbers are often identical. This will help to reduce the confusion.
VERY CLEVER AND EASY.
HELPED ME ACTUALLY GET A BETTER FEELING FOR HOW OUT OF RANGE MY PATIENT’S BS’S ARE.
MOST PATIENTS USE APPS NOW AND THIS IS SO EASY FOR THEM TO RELATE TO.
It will provide data for better compliance.
Wondering if Readers have suggestions for a good App re: antibiotic therapy and guide.
“Mark my words – the day is not far off when physicians will be prescribing patients Smartphone apps and wearable sensor devices just as routinely as they prescribe pharmaceuticals, physical therapy and other treatment options today.
Ambulatory patient monitoring is one example of a clinical diagnostic technology that is on the verge of achieving full mobilization via consumer Smartphone devices and wearable sensors. Traditionally this technology could only be used with a high degree of reliability in a clinical setting. However, Wireless Body Area Network (WBAN) technologies are enabling clinicians to remotely monitor patients in real-time and even provide biofeedback to patients based on each individual’s personal physiological data, all via Smartphones.”
Article
Brian Edwards, iMedicalApps, 11 August 2011
Was asked recently to nominate my essential apps: this is the list I came up with
My most used
Evernote: for little snippets of information. Syncs with desktop application
Dropbox: for syncing files with desktop dropbox folder
These two are my must haves.
I use Mediquations for things like the opioid calculator and others.
OB patients for tracking my mat pts.
HanDbase for my billing, obstetric log (unfortunately OB patients won’t log the pt once delivered) and field notes (amongst other things).
Talking Tom and Talking Carl to try and convince recalcitrant toddlers to let me look in their ears.
RDP to use my EMR over VPN (how’s that for TLAs?!)
The BC guidelines app of course
And the TRes app of course:)
Still trying to decide between PALS CoreChart and PediStat. Problem is don’t get call to use all that often to really test.
Dermatomes cause I can never flippin remember them!
The Americans frequently use the HbA1C as a screening tool for diabetes which to me seems quite logical. You do not need to be fasting and it quite conveniently can be included along with other lab requests at the same time. However, as everyone knows up here in BC, MSP technically does not cover this test to be used as a screening tool.
I do not encourage my T2DM to self monitor their blood sugars. The cost to the taxpayer is substantial in comparison to a 3/12 A1C. I do show them the correlation between mmol readings and the A1C percentage if they do have BSM.
Daniel Kraft: Medicine’s future? There’s an app for that http://www.ted.com/talks/daniel_kraft_medicine_s_future.html
Excellent persuasive tool. I will start using it immediately. Diabetics all seem to have problems understanding the hba1c and how it correlates to there home readings
good argument to get a smartphone!
Useful. Now if we can just get wireless in hospital…
Since I am using an EMR on a Windows computer, I would find it more helpful to have a Windows application that would be the equivalent of the iPhone app – or use a spreadsheet to calculate the conversion