Author
Sander Veldhuyzen van Zanten, MD, FRCPC, MSc, MPH, PhD (biography and disclosures)
Disclosures: No disclosures relevant to this publication. Received peer and non-peer-reviewed funding for clinical studies of Helicobacter infection in the past. Received speaker fees and member of advisory boards for H. pylori related activities. None in the last five years. Mitigating potential bias: Only published trial data is presented. Recommendations are consistent with published Canadian and International guidelines (references 4-7). Recommendations are consistent with current practice patterns.
What gaps I have noticed
Helicobacter pylori (H. pylori) continues to be an important pathogen associated with peptic ulcer disease, dyspepsia, and gastric cancer.
Data that answers these gaps
The epidemiology of H. pylori in Canada is changing.1 It can now rarely be found in second-generation Canadians, but the prevalence continues to be high in immigrants, children of immigrants, and First Nations Canadians. In an H. pylori positive individual the lifetime risk of developing gastric or duodenal ulcers is 5 to 15% and dyspepsia up to 25%. H. pylori is an important risk factor for development of gastric cancer, but this is rare, occurring in less than 1 in 1,000 infected individuals. Most infections are acquired in childhood, during the first 5–10 years of life.2,3 In a substantial proportion of individuals, the infection remains dormant and causes no symptoms. Although most H. pylori infections are acquired in childhood, it is not recommended to routinely test family members of H. pylori infected individuals. Among adults, it is very unlikely that H. pylori is transmitted, even when there is close personal contact.
Worldwide and in Canada the guidelines for the treatment of H. pylori infection changed in 2016.4-7 Details of the medications used, the dosages, and frequencies, are listed in Table 1. Importantly, the recommended duration for most regimens is 14 days.
What I recommend (practice tips)
Who should be tested for Helicobacter and how?
Generally speaking, do not test patients for H. pylori unless you are prepared to treat if they are positive.
Patients who should be tested for H. pylori:
- Duodenal or gastric ulcer diagnosis (recent or in the past)
- Dyspepsia (epigastric pain dominant symptoms)
- First-degree family history of gastric cancer (especially if index case is young)
- High-risk groups (First Nations, immigrants)
H. pylori can be diagnosed by histology when biopsies are taken during gastroscopy. The urea breath test (UBT) is a very accurate and robust test to diagnose the infection.8 More recently, the H. pylori stool antigen test (HpSAT) has been used more frequently.9 It is an accurate test but it has a higher proportion of equivocal results than the UBT. Use of serology to detect H. pylori infection is not recommended as it cannot discriminate between a current active infection or an old (treated) infection in the past. Importantly, one has to stop PPIs (proton pump inhibitors) for 14 days prior to performing a urea breath test or HpSAT. The reason is that up to 20% of people while on PPIs may get false negative results due to suppression of the organism by the PPI.10
Although a large proportion of patients with duodenal or gastric ulcers are H. pylori positive, H. pylori negative ulcers are becoming more common. Therefore, it is recommended to document that a patient is H. pylori positive before initiating treatment. The most common cause of H. pylori negative ulcers are NSAIDs and antiplatelet agents.
Helicobacter treatment recommendations have changed
The conventional triple combination of a PPI, clarithromycin (Cl), and either amoxicillin (A) or metronidazole (Met) is no longer recommended because its success rates have decreased to less than 60%.11,12 This includes the use of Hp-PAC®, the combination of lansoprazole, amoxicillin, and clarithromycin.
Recommended treatments (summarized in Table 1 below):
- The new recommended first-line therapy is called concomitant or ClAMet (using the initials of clarithromycin (Cl), amoxicillin (A), and metronidazole (Met)) given for 14 days.4-7 Its efficacy is 80–85%.
- The best second-line therapy is bismuth-based quadruple therapy (PPI, bismuth, metronidazole, and tetracycline) given for 14 days. The higher dose of metronidazole 500 mg is the author’s preference as there is evidence that it can better overcome partial resistance to metronidazole.13 This is a robust treatment that can also be used as first line. The downside of bismuth-based quadruple therapy (Bi-Quad) is that it is a complex regimen consisting of up to 24 pills a day. Some of the medications need to be taken twice and others four times a day. Bi-Quad also has more side effects than concomitant therapy.
- The third-line therapy is the combination of a PPI, amoxicillin, and levofloxacin (PPI-AL) given for 14 days. The author uses the higher dose of levofloxacin 500 mg bid. Sometimes PPI-AL is given as second line instead of Bi-Quad because it is an easier regimen to take, but it is less well tested. PPI-AL should not be used as first-line therapy because the background rate of levofloxacin resistance is high in Canada, up to 15%.14 This high rate is likely explained by the high use of fluoroquinolones for other indications.
- There is a fourth-line therapy consisting of a PPI with amoxicillin and rifabutin (Rif). In Canada, its efficacy is 62% when given as rescue therapy.15 This is the only therapy for which the duration is 10 days instead of 14 days. However, family physicians may want to consider referring patients to a GI specialist should the three first-choice therapies have failed. Use of rifabutin often needs special authorization. In the USA, a combination tablet of omeprazole, amoxicillin, and rifabutin (Talicia), has been available since 2019. It has been tested as a first-line therapy and the success rate of 10-day therapy was 84%.16 The tablet is not available in Canada and the decision to move the PPI-amoxicillin-rifabutin combination to first line requires more studies.
If the above-listed four therapies are given in sequence to individuals who failed higher order therapies (i.e., start with concomitant, followed by B-Quad, etc.) the cumulative success rate is 96–97%.17, 18 The first choice of therapy in patients with a true penicillin allergy is Bi-Quad. If that fails, the second line of therapy is triple therapy with PPI, Clarithromycin, and Metronidazole (PPI-CM) given for 14 days.4
One thing to note, although there are pharmacologic differences among the different PPIs, resulting in differences in acid suppression19, for day-to-day practice PPIs, when given in standard doses, are generally considered equal when treating common conditions such as Gastro Esophageal Reflux Disease (GERD) or peptic ulcer disease (PUD). For treatment of H. pylori, there is some evidence that using the more potent PPIs, such as esomeprazole or rabeprazole, slightly higher success rates are achieved compared to pantoprazole.20
What patients need to know about the treatments
It is important that patients get a clear explanation about these treatments, preferably with a handout. Examples of handouts the author uses about the importance of H. pylori infection and the different treatments are available in the patient handouts section below. Prescribing anti-Helicobacter therapy is difficult to do well over the phone. It is helpful for patients to prescribe these treatments in a blister pack, as the regimens are complex. That way patients are not confused about which medications have to be taken and when. Patients should be told that compliance is very important as cure rates drop significantly if treatments are not taken for the full duration. See handouts for patients.
Is it necessary to test whether the treatment was successful?
It is generally recommended to test whether treatment was successful. In primary care, UBT or the stool antigen test are used for this. Importantly, one has to wait at least 4 weeks after the treatment was finished before re-testing is done to avoid getting false negative results. Once again, it is important that PPI therapy, if there is an ongoing need for it after the antibiotics are finished, is held for 14 days prior to the repeat testing for Helicobacter.10 Patients can be managed during those 14 days with standard doses of antacids if they have symptoms while off the PPI. If the patient is negative after appropriate testing for cure was done, it is very unlikely such a patient will get re-infected later in life. In adults, most patients who are thought to have a re-infection, in fact, have a false negative test result in the past. They usually have recrudescence of their original H. pylori strain.21
Given that none of the current H. pylori therapies are 100% successful it is my practice to always test whether cure has been received after each treatment. I generally give a patient three or four rounds of treatment if needed but I should state that I have a special interest in H. pylori. What to do with patients who fail more than four therapies should be decided on a case-by-case basis. This may in part depend on the indication for treatment. An option is to refer the patient for antibiotic resistance testing for which a gastroscopy is required. Knowledge of the resistance pattern on the strain may guide further therapy. However, testing of H. pylori strains is not widely available in Canada and data on resistance are scarce. The data show that resistance to clarithromycin and metronidazole and also levofloxacin is high. Resistance to amoxicillin and tetracycline is rare.4,14, 22-24
Another management option is the decision not to treat Hp any further, but possibly observe these patients long-term. Long-term follow-up especially is a consideration, if there is a family history of gastric cancer or if more severe gastric metaplasia was present on histology.25,26
Peptic ulcer disease
There are a few important recommendations in the management of patients diagnosed with acute peptic ulcer disease (duodenal or gastric ulcers), and especially bleeding ones, for example during a hospitalization. If they turn out to be H. pylori positive it is important to continue PPI therapy after the 14-day anti-Helicobacter treatment, for at least 8–16 weeks, to ensure adequate healing of the ulcer. Importantly, in such patients, the PPI should not be stopped until there is proof that the H. pylori infection has been successfully cured. The reason for this is that should treatment have failed to cure H. pylori, these patients are at risk of getting recurrent ulceration (with possible bleeding) if PPI maintenance therapy is not given.27 A decision whether or not to continue PPI longer term should only be taken once cure of H. pylori has been established.
There is evidence that anti-Helicobacter therapy is effective in the treatment of H. pylori positive gastric or duodenal ulcers. However, a proportion of such patients will require long-term PPI therapy because of ongoing symptoms even though H. pylori was cured. Another reason for ongoing acid-suppressive therapy may be that some of these patients, especially older ones (> 65–70 years) require, for example, anticoagulation and/or antiplatelet agents for management of cardiovascular risk factors. Given that they, therefore, have an ongoing risk of developing (bleeding) ulcers it is reasonable to maintain such patients on a once-a-day PPI for ulcer prophylaxis.
The role of Helicobacter in dyspepsia and GERD
There is definite evidence that a test and treat strategy for H. pylori is efficacious in patients who present with dyspepsia symptoms in primary care.28 Dyspepsia is defined as epigastric pain or discomfort which may be accompanied by other upper GI symptoms, such as burning sensation or excessive burping. Compared to no-antibiotic treatment, more patients will have permanent resolution of their dyspepsia symptoms following cure of the H. pylori infection. However, clinical trial data, including studies from Canada, have shown that more than 50% of dyspepsia patients will have ongoing dyspepsia symptoms, often requiring acid suppressive therapy, after successful cure of the infection.28
Another important comment on the management of dyspepsia is that there is good evidence that PPIs work in epigastric pain dominant dyspepsia (ulcer-like dyspepsia), and in those who have concomitant symptoms of heartburn (reflux-like dyspepsia). However, PPIs are generally not effective in so-called dysmotility-like dyspepsia where upper abdominal bloating rather than epigastric pain or discomfort is the dominant symptom.29 In this subgroup of patients, PPIs do not provide benefits. In such patients overlap with possible IBS or other diagnoses needs to be further explored.
In Canada nowadays, gastroesophageal reflux disease (GERD) is more common than dyspepsia. The diagnosis of GERD can be made based on the presence of dominant symptoms of heartburn and/or regurgitation.30 Importantly the clinical course of GERD (frequency of symptoms, need for acid suppressive therapy) will not be altered by successful cure of a coexisting H. pylori infection.31 It is important to tell patients about this as most of them will require ongoing maintenance therapy with PPI for control of their GERD symptoms even though H. pylori has been cured. For this reason, it is not recommended to routinely test for H. pylori at the time GERD is diagnosed in patients. This is in contrast to the patient who has dyspepsia, defined by epigastric pain or discomfort as the dominant symptom rather than heartburn, where a test for Helicobacter is recommended.30
The incidence of gastric cancer has been decreasing for decades in Canada but it is still more common than esophageal cancer. 32 Apart from smoking, presence of H. pylori is the only other main modifiable risk factor for gastric cancer. It is recommended that all 1st degree relatives of gastric cancer patients are tested and, if positive, treated for Helicobacter, especially if the index case occurred at a younger age.25,32 The risk of gastric cancer is much higher in First Nations people compared to the average Canadian population33,34,35 and the high prevalence of H. pylori is likely a partial explanation for this. The prevalence of H. pylori is also high in immigrants from certain areas, such as Southeast Asia and Central and South America. In those patients, one should have a low threshold to test for H. pylori infection. In general, in children, who have a 1st degree relative with gastric cancer, the recommendation is to wait with testing and treatment until after they have gone through puberty.
Table 1. The most commonly used treatments for H. pylori infection
| Treatment | Medications |
| Concomitant Therapy (ClAMET) |
|
| Bismuth-based Quadruple Therapy (Bi-Quad) |
|
| PPI-Amoxicillin-Levofloxacin (P-AL) |
|
| Rifabutin-based Triple Therapy (P-A-Rif) |
|
| Treatments that no longer should be used: | |
| PPI-CA Triple Therapy |
|
| PPI-CM Triple Therapy |
|
- Proton Pump Inhibitor=PPI. Options: Omeprazole 20mg, Pantoprazole 40 mg, Lansoprazole 30 mg, Rabeprazole 20mg, Esomeprazole 40mg, Dexlansoprazole 60mg
- Cl=Clarithromycin
- M= Metronidazole
- A= Amoxicillin
- B= Bismuth subsalicylate
- T= Tetracycline
- L=Levofloxacin
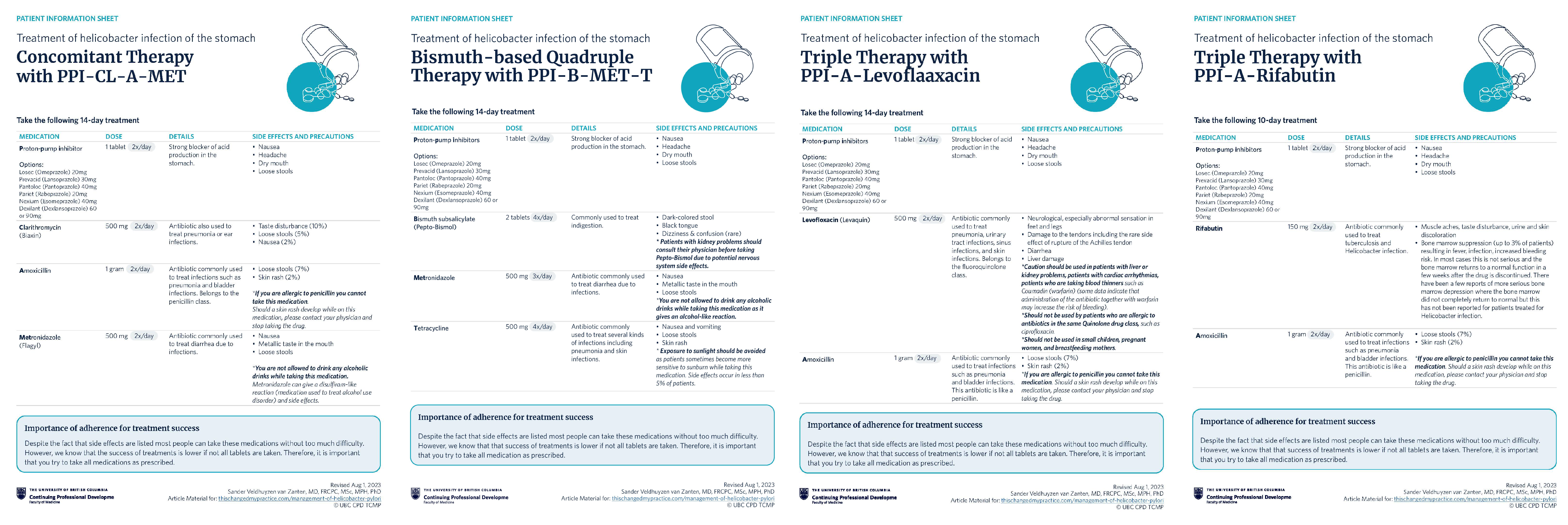
Handouts for patients
- Helicobacter infection of the stomach
- Concomitant Therapy (CLAMET)
- Bismuth-based Quadruple Therapy (Bi-Quad)
- PPI-Amoxicillin-Levofloxacin Therapy (P-AL)
- Rifabutin-based Triple Therapy (P-A-Rif)
References
- Veldhuyzen van Zanten SJ, Pollak PT, Best LM, Bezanson GS, Marrie T. Increasing prevalence of Helicobacter pylori infection with age: continuous risk of infection in adults rather than cohort effect. J Infect Dis. 1994;169(2):434-437. doi:10.1093/infdis/169.2.434 (Request with CPSBC or view with UBC)
- Hooi JKY, Lai WY, Ng WK, et al. Global prevalence of Helicobacter pylori infection: systematic review and meta-analysis. Gastroenterology. 2017;153(2):420-429. doi:10.1053/j.gastro.2017.04.022 (View)
- Malaty HM, El-Kasabany A, Graham DY, et al. Age at acquisition of Helicobacter pylori infection: a follow-up study from infancy to adulthood. Lancet. 2002;359(9310):931-935. doi:10.1016/S0140-6736(02)08025-X (View with CPSBC or UBC)
- Fallone CA, Chiba N, van Zanten SJO, et al. The Toronto consensus for the treatment of Helicobacter pylori infection in adults. Gastroenterology. 2016;151(1):51-69.e14 (Request with CPSBC or view with UBC)
- Chey WD, Leontiadis GI, Howden CW, Moss SF. ACG clinical guideline: treatment of Helicobacter pylori Infection [published correction appears in Am J Gastroenterol. 2018 Jul;113(7):1102]. Am J Gastroenterol. 2017;112(2):212-239. doi:10.1038/ajg.2016.563 (View with CPSBC or UBC)
- Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht V/Florence consensus report. Gut. 2017;66(1):6-3. (View)
- Malfertheiner P, Megraud F, Rokkas T, et al. Management of Helicobacter pylori infection: the Maastricht VI/Florence consensus report. Gut. 2022;gutjnl-2022. doi:10.1136/gutjnl-2022-327745 (View)
- Chiba N, van Zanten SJO. 13C-Urea breath tests are the non-invasive method of choice for Helicobacter pylori detection. Can J Gastroenterol. 1999;13(8):681-683. doi:10.1155/1999/683452 (Request with CPSBC or view with UBC)
- Best LM, Takwoingi Y, Siddique S, et al. Non-invasive diagnostic tests for Helicobacter pylori infection. Cochrane Database Syst Rev. 2018;3(3):CD012080. doi:10.1002/14651858.CD012080.pub2 (View)
- Graham DY, Opekun AR, Hammoud F, et al. Studies regarding the mechanism of false negative urea breath tests with proton pump inhibitors. Am J Gastroenterol. 2003;98(5):1005-1009. doi:10.1111/j.1572-0241.2003.07426 (View with CPSBC or UBC)
- Graham DY, Fischbach L. Helicobacter pylori treatment in the era of increasing antibiotic resistance. Gut. 2010;59(8):1143-1153. doi:10.1136/gut.2009.192757 (Request with CPSBC or view with UBC)
- Rodgers C, van Zanten SV. A meta-analysis of the success rate of Helicobacter pylori therapy in Canada. Can J Gastroenterol. 2007;21(5):295-300. doi:10.1155/2007/419784 (View)
- Dore MP, Lu H, Graham DY. Role of bismuth in improving Helicobacter pylori eradication with triple therapy. Gut. 2016;65(6):870-878. doi:10.1136/gutjnl-2015-310084 (Request with CPSBC or view with UBC)
- Best L, Cooper-Lesins G, Haldane D, Veldhuyzen van Zanten SJO. Helicobacter pylori antibiotic resistance in Canadian populations (abstr S1293). Gastroenterology. 2004;126:S1293. A-189 (View, pg 46)
- van Zanten SV, Desai S, Best L, et al. Rescue therapy using a rifabutin-based regimen is effective for cure of Helicobacter pylori infection. Can J Gastroenterol. 2010;24(5):303-306. doi:10.1155/2010/637908 (View)
- Graham DY, Canaan Y, Maher J, Wiener G, Hulten KG, Kalfus IN. Rifabutin-Based Triple Therapy (RHB-105) for Helicobacter pylori eradication: a double-blind, randomized, controlled trial. Ann Intern Med. 2020;172(12):795-802. doi:10.7326/M19-3734 (Request with CPSBC or view with UBC)
- Buttenschoen J, D’Souza P, Veldhuyzen van Zanten S. Cumulative results of Helicobacter pylori therapy using sequential therapy, bismuth quadruple therapy, levofloxacin-based triple therapy, and other regimens. Can J Gastroenterol Hepatol. 2016;30(Suppl A):A-229. doi: 10.1155/2016/4792898 (View)
- Krahn T, van Zanten S. A142 Trends in Helicobacter pylori treatment and cure in Edmonton: 2015-2020. J Can Assoc Gastroenterol. 2021;4:129-131 (View)
- Graham DY, Tansel A. Interchangeable Use of proton pump inhibitors based on relative potency. Clin Gastroenterol Hepatol. 2018;16(6):800-808.e7. doi:10.1016/j.cgh.2017.09.033 (View)
- Fernández-Salazar L, Campillo A, Rodrigo L, et al. Effectiveness and safety of high-dose dual therapy: results of the European registry on the management of Helicobacter pylori infection (Hp-EuReg). J Clin Med. 2022;11(12):3544. Published 2022 Jun 20. doi:10.3390/jcm11123544 (View)
- Xia HX, Windle HJ, Marshall DG, Smyth CJ, Keane CT, O’Morain CA. Recrudescence of Helicobacter pylori after apparently successful eradication: novel application of randomly amplified polymorphic DNA fingerprinting. Gut. 1995;37(1):30-34. doi:10.1136/gut.37.1.30 (View)
- Best LM, Haldane DJ, Bezanson GS, Veldhuyzen van Zanten SJ. Helicobacter pylori: primary susceptibility to clarithromycin in vitro in Nova Scotia. Can J Gastroenterol. 1997;11(4):298-300. doi:10.1155/1997/159637. (Request with CPSBC or view with UBC)
- Fallone CA. Epidemiology of the antibiotic resistance of Helicobacter pylori in Canada. Can J Gastroenterol. 2000;14(10):879-882. doi:10.1155/2000/562159 (Request with CPSBC or view with UBC)
- Morse AL, Goodman KJ, Munday R, et al. A randomized controlled trial comparing sequential with triple therapy for Helicobacter pylori in an Aboriginal community in the Canadian North [published correction appears in Can J Gastroenterol. 2014 Mar;28(3):167]. Can J Gastroenterol. 2013;27(12):701-706. doi:10.1155/2013/143047 (View)
- Choi IJ, Kim CG, Lee JY, et al. Family History of gastric cancer and Helicobacter pylori treatment. N Engl J Med. 2020;382(5):427-436. doi:10.1056/NEJMoa1909666 (Request with CPSBC or view with UBC)
- Gupta S, Li D, El Serag HB, et al. AGA Clinical Practice Guidelines on Management of Gastric Intestinal Metaplasia. Gastroenterology. 2020;158(3):693-702. doi:10.1053/j.gastro.2019.12.003 (View)
- Chan FK, Chung SC, Suen BY, et al. Preventing recurrent upper gastrointestinal bleeding in patients with Helicobacter pylori infection who are taking low-dose aspirin or naproxen. N Engl J Med. 2001;344(13):967-973. doi:10.1056/NEJM200103293441304 (View)
- Chiba N, Van Zanten SJ, Sinclair P, Ferguson RA, Escobedo S, Grace E. Treating Helicobacter pylori infection in primary care patients with uninvestigated dyspepsia: the Canadian adult dyspepsia empiric treatment-Helicobacter pylori positive (CADET-Hp) randomised controlled trial. BMJ. 2002;324(7344):1012-1016. doi:10.1136/bmj.324.7344.1012 (View)
- Moayyedi P, Delaney BC, Vakil N, Forman D, Talley NJ. The efficacy of proton pump inhibitors in nonulcer dyspepsia: a systematic review and economic analysis. Gastroenterology. 2004;127(5):1329-1337. doi:10.1053/j.gastro.2004.08.026 (Request with CPSBC or view with UBC)
- Veldhuyzen van Zanten SJ, Flook N, Chiba N, et al. An evidence-based approach to the management of uninvestigated dyspepsia in the era of Helicobacter pylori. Canadian Dyspepsia Working Group. CMAJ. 2000;162(12 Suppl):S3-S23 (View)
- Moayyedi P, Bardhan C, Young L, Dixon MF, Brown L, Axon AT. Helicobacter pylori eradication does not exacerbate reflux symptoms in gastroesophageal reflux disease. Gastroenterology. 2001;121(5):1120-1126. doi:10.1053/gast.2001.29332 (Request with CPSBC or view with UBC)
- Canadian Cancer Statistics Advisory Committee in collaboration with the Canadian Cancer Society, Statistics Canada and the Public Health Agency of Canada. Canadian Cancer Statistics 2021. Toronto, ON: Canadian Cancer Society; 2021. Accessed July 31, 2023 (View)
- Goodman KJ, Jacobson K, Veldhuyzen van Zanten S. Helicobacter pylori infection in Canadian and related Arctic Aboriginal populations. Can J Gastroenterol. 2008;22(3):289-295. doi:10.1155/2008/258610 (View)
- Cheung J, Goodman K, Munday R, et al. Helicobacter pylori infection in Canada’s Arctic: searching for the solutions. Can J Gastroenterol. 2008;22(11):912-916. doi:10.1155/2008/614538 (View)
- Colquhoun A, Hannah H, Corriveau A, et al. Gastric Cancer in Northern Canadian Populations: A focus on cardia and non-cardia subsites. Cancers (Basel). 2019;11(4):534. Published 2019 Apr 15. doi:10.3390/cancers11040534 (View)
PathwaysBC Resources
Helicobacter pylori associated duodenal/gastric ulcer: adult patient treatment recommendations. Bugs & Drugs. Accessed July 19, 2023. https://pathwaysbc.ca/ci/1886
Patient handouts for tests, emailable via PathwaysBC:
- Patient instructions: Helicobacter pylori stool antigen test. LifeLabs. Accessed July 19, 2023. https://pathwaysbc.ca/ci/5953
- Patient instructions: Helicobacter pylori urea breath test. LifeLabs. Accessed July 19, 2023. https://pathwaysbc.ca/ci/1977

In Ontario h.pylori breath test and fecal testing is private pay rendering it inaccessible to the majority of newcomers especially the refugee population.
We are left with serology which as pointed out will always remain positive.
The proposed strategy of retesting for cure after treatment renders this even more challenging to use this approach.
Otherwise a good overview and review.
Thank you for this excellent TCMP! You specify that the PPI should not be stopped in patients with H Pylori confirmed PUD (and especially bleeding ulcers) until the infection is confirmed eradicated – but I presume one must stop the PPI for 14 days in order to completed a UBT or HpSAT to confirm successful treatment? i.e. continue a PPI for 8-12 weeks after the 14 day eradication period, and then stop it for 2 weeks prior to testing the patient again?
I agree with the change to quad therapy as first line treatment.
In Sask as well I believe it is not easy access to get the urea breath test, however, stool antigen is much more accessible.
I am curious about the need to hold a PPI prior to the stool antigen or endoscopy as to what the percentage of equivocal results would be?
For Joanne in Ontario, I do hope the province moves to cover at least stool antigen as a much less invasive way than endoscopy for getting results that are not private pay.
If someone has ulcers confirmed by endoscopy my referral centre will treat empirically and after treatment will continue minimum 3 months of PPI
I think as well telling patients the pill burden before they pick up the prescription is important to increase compliance as it is a lot of medications for two weeks to take, and I have had some people say they didn’t finish the course as it was to many pills!
Very relevant TCMP, thank you!
While I was practicing as a GP Anesthetist, and taking an NSAID for shoulder pain, I had a GI bleed. I was H Pylori positive on gastroscopy. I had the multi pill regime.
Since then, if I have spicy pizza and/or a beer, I get some indigestion, and will take a PPI for a few days. Likely about 7 tablets per month, on average.
Is being an anesthetist still considered a risk factor for IPylori infections?
Begs the question of whether I should be worked up again.? Gastroduodenosopy. Or, whatever.
KP born 1945.
BSc (Hons. Chem) MD CCFP FCFP LM
Clinical Associate Professor, Retired
Department of Family Practice,
Faculty of Medicine, University of BC
Thank you- good update for current treatment approach – also should mention diet and eliminating caffeine – esp the AM caffeine – on empty stomachs
Great presentation on current approach to treatment of H.pylori ; still dispense a lot of HP-PAC combos and occasionally get the Bi-QUAD therapy dispensed.
Thanks for a great review of H Pylori testing and treatment. Will use the blister packs! I anticipate it will still be a challenge for me to differentiate patients with dyspepsia vs GERD. Any further tips on this?
Thanks for coming up with this amazing piece on the subject. Can you please advise on which foods to take and avoid while treating H. Pylori?
@ Mairead Keady: Yes that is correct. I would continue to treat with PPI for at least 3 months if indeed an ulcer was seen. After that one can usually hold the PPI for 2. Weeks. This assumes the patient does not have any ongoing dyspepsia symptoms. Sometimes if the patient has heartburn symptoms that are troublesome one can give antacids temporarily
@ Evan M: The issue is false negative or equivocal results. If an endoscopy is done there is no need to hold the PPI as histology generally will detect Hp if the infection is persistent. Importantly biopsies need to be taken from both the antrum AND the body part of the stomach to avoid false negative results.
For UBT and stool antigen test the recommendation is to hold PPIs for 14 days prior to the test. The stool test has more equivocal results than the UBT. Not much data have been published on the rates of equivocal or false negative results.
@ R Keith Phillips: Endoscopists and possibly anesthesiologists were reported to have a higher risk of Hp infection but there are no recent data on this. It is recommended to repeat testing to determine whether Hp was cured after Hp treatment is given. This is especially true if one had a bleeding ulcer. In this case was there indeed a bleeding ulcer seen as the cause of the GI bleed? In this case the NSAID may have triggered the GI bleed but test for cure of Hp is still recommended. I do not think it likely that the spicy food is the cause of the upper GI symptoms. More likely this is due to underlying GERD (heartburn dominant symptom) or dyspepsia (epigastric discomfort dominant symptom). In this case given there is frequent recurrence of symptoms I would consider taking a PPI every day. And this even more so since there is a history of a previous upper GI bleed.
@Dr. Cynthia L. Clark: Any further tips on to differentiate patients with dyspepsia vs GERD? Not really. Importantly PPIs are effective in both conditions. There is a lot of overlap between GERD and Dyspepsia. In GERD heartburn is often the dominant symptom. In dyspepsia epigastric pain or discomfort is the dominant symptom. If gastroscopy is done in patients with dyspepsia reflux esophagitis is more commonly seen than gastric or duodenal ulcers. So GERD is more common.
@Ron Abraham A healthy diet is very important. And so is quitting smoking as this is a risk factor for GERD, peptic ulcers and upper GI bleeding. I never take people off a good cup of coffee! (I myself love a cappuccino in the morning and would not comply with stopping having them) But excessive intake of coffee can cause indigestion.
Does the quad-pack come prepacked like H-pak or would it be better to get the pharmacist to bubble pack for better adherence?
Thanks
Mary Obstfeld, NP
Cold Lake First Nations, Alberta
Brilliant brilliant paper on Pylori infection
I have 2 questions and will be most grateful if you could share some answers;
1, what do you do if you started treating a patient for infective diarrhea before getting your stool for Pylori antigen results, will you advise that the patient completes the course of the 1st antibiotic before starting the quad therapy, or discontinue and start the quad therapy?
2. Can l also request a stool routine examination as well when I am suspecting H Pylori infection?
Thank you so much.
Does the quad therapy also apply to children managed for Pylori infection?