Authors
- John van Bockxmeer, MBBS, CCFP (biography, no disclosures)
- Vishal Varshney, MD, FRCPC (biography and disclosures)
- Anthony Lau, PharmD, ACPR, BCPS (biography, no disclosures)
Dr. Vishal Varshney disclosures: Received honoraria from Medtronic Abbott. Mitigating potential bias: Treatments or recommendations in this article are unrelated to products/services/treatments involved in disclosure statements. Only published trial data is presented. Recommendations are consistent with current practice patterns.
What I did before
When treating patients for acute inflammatory and musculoskeletal pain in the urgent primary care clinic or outpatient setting, I would use medication doses within the upper ranges suggested by common physician resources such as the BC Guidelines.1 I often titrated nonsteroidal anti-inflammatory drugs (NSAIDs) based on my patient’s pain response to maximum total daily doses of 3 g of ibuprofen and 40 mg of ketorolac in healthy adults aged up to 65 years with normal renal function. I would also prescribe as-needed doses for nurses to administer 600 mg of oral ibuprofen and 30 mg of intramuscular (IM) ketorolac.
What changed my practice
I recently became increasingly aware of the international expert emergency medicine opinion, which highlighted the need for more judicious NSAID prescribing. During a BC rural locum assignment, I witnessed upper gastrointestinal bleeding (UGIB), which I believe could have been preventable. The young patient had been self-administering oral ibuprofen for a week after suffering a skiing injury. The dose they used was within guidelines and the patient had no other chronic medical conditions, but concurrently consumed alcohol. I had wondered if health-care providers utilizing similar doses were unintentionally causing UGIBs while providing minimal additional analgesia. I thus began discussing this topic with my co-authors and we researched the concept of pharmacological ceiling effects of NSAID medications.
All medications have therapeutic windows with target range concentrations balancing efficacy and toxicity. Some analgesic drugs such as NSAIDs have inherent ceiling concentrations beyond which additional doses offer no analgesic benefit and potentially increased adverse events. NSAIDs inhibit both cyclooxygenase-1 (COX-1) and inducible cyclooxygenase-2 (COX-2). Non-selective NSAIDs inhibit COX-1 enzymes, while COX-2 inhibitors, such as celecoxib, preferentially block COX-2 enzymes in different areas of the body. Since COX-1 enzymes are expressed in the gastric mucosa, non-selective NSAIDs pose a higher GIB risk than COX-2 inhibitors. However, both types exhibit ceiling doses. These rate-limiting enzymes are responsible for the synthesis of prostaglandins and thromboxane involved in modulating pain signalling and inflammation development respectively.2 At ceiling doses, the COX enzyme activity sites become saturated with the NSAID. No free enzymes can bind to further added substrates, producing a plateauing effect of the drug’s efficacy. Increasing doses beyond this point produces higher concentrations of free drug which is unable to bind to the saturated COX isoenzymes, resulting in no additional therapeutic benefit and only increased risk of harm. The risk of adverse effects is dependent on where the COX isoenzymes are found. Non-selective NSAIDs have higher GIB risk due to COX-1 inhibition in the gastric mucosa cells. Whereas, COX-2 inhibitors have higher risk of myocardial infarction and stroke due to unopposed thromboxane A2-induced vasoconstriction and platelet aggregation from COX-2 enzyme suppression.3
Conceptually, ceiling doses are important to be aware of because common NSAIDs such as ketorolac and ibuprofen are prescribed at higher doses in many settings. Several published studies support my approach of utilizing the lowest effective analgesic ceiling doses for ketorolac and ibuprofen in my clinical practice.
Motov et al. conducted a randomized double-blinded trial comparing oral ibuprofen dosed at 400, 600, and 800 mg for acute pain management in adult patients in an emergency department setting.4 They found the reduction in pain scores within 60 minutes and adverse effect rates amongst all three treatment groups to be similar. Based on this discussion, it appears that 400 mg may be the analgesic ceiling dose for ibuprofen when given to patients in the emergency department for common causes of acute pain. Doses beyond this would unlikely provide any additional analgesic effect.
For clinicians preferring to prescribe naproxen, ceiling dose data may be more nuanced and unclear. The Oxford League Table suggests a ceiling dose of 440 mg beyond which there is no additional benefit but increased adverse reactions.5 This was based on efficacy data reducing moderate-severe post-operative pain scores by 50%. The Number Needed to Treat (NNT) to achieve this was 3.1, 2.3, and 3.0 for common doses of 220/250 mg, 440 mg, and 500 mg respectively. The challenge with this evidence is that relative efficacies of doses were similar, confidence intervals overlapped, and figures were derived from studies comparing a variety of pain modalities in different patient groups. If naproxen is used the authors’ recommendation is to dose 250–375 mg po BID.
Motov et al. also compared intravenous ketorolac 10, 15, and 30 mg IM for moderate to severe acute pain management, finding no significant differences in pain reduction, pain scores, and rates of rescue analgesia between the different doses.6 Noninferiority of ketorolac dosing has also been demonstrated in other clinical contexts including chronic oncological pain, acute gynaecological surgery, and spinal and surgical post-operative environments.7, 8, 9, 10 IM/IV doses typically compared in these studies range between 10 and 90 mg of ketorolac.
One study sought to explore the combination of various IV ketorolac dosing regimens (5, 7.5, 10, 12.5, 15, or 30 mg administered every 6 h) and PCA morphine in patients who underwent spinal fusion.10 The total dose of morphine required and patient-reported pain scores were significantly higher in the 5 mg ketorolac group. I, therefore, consider using a minimum dose of 7.5 mg of ketorolac, acknowledging its noninferiority to higher doses.
When reviewing the onset of action, I inform my patients that analgesia can last for six hours following the administration of the lower 10 mg ketorolac dose. This is corroborated by a trial by Minotti et al. comparing 10 and 30 mg doses of ketorolac and diclofenac 75 mg for management of acute moderate to severe cancer pain.11 In this study, approximately 70% of all treatment groups achieved and maintained adequate pain control throughout the 6-hour monitoring period with no significant difference in pain intensity scores.
While the analgesic effects of ketorolac and ibuprofen plateau at their ceiling doses, bleeding risk is dose-dependent with an increased risk proportional to dose increases. This dose-dependent relationship in the NSAID adverse effect profile was demonstrated in a study by García Rodríguez et al.12 The authors found that the risk of UGIB and/or perforation significantly increased with higher daily doses of NSAIDs. Of particular note, patients receiving ketorolac presented with the highest UGIB risk which was measured to be five times more gastrotoxic than all other NSAIDs. In this study, the authors ascertained a dose-dependent relationship for ketorolac’s UGIB risk whereby daily doses less than or equal to 20 mg were associated with an adjusted risk ratio of 20.0, and daily doses greater than 20 mg were attributed to an adjusted risk ratio of 28.1.
Evidence for optimal therapeutic duration of NSAIDs is informed by an FDA black box warning for a five-day maximum for ketorolac. A 1996 post-marketing surveillance study published in JAMA by Strom et al. established a duration-dependent effect on GI bleeding risks. Ketorolac use of greater than 5 days approximately doubled the risk of GI bleeds compared to those without ketorolac (OR 2.20; 95% CI 1.36–3.57).13 The authors concluded that by limiting ketorolac treatment to patients under 65 years of age at a maximum dose of 10 mg/day and duration of five days, the risk of GI and operative site bleeding would not increase (OR 1.03; 95% CI 0.80–1.34 and OR 0.90; 95% CI 0.82–0.98 respectively). A case-control study found 6 days or less was not associated with increased GI lesion formation.14 Menniti-Ippolito et al. associated significant rates of GI lesion formation, hemorrhage, or perforation with ketorolac use over a median of six days compared to other NSAIDs.15
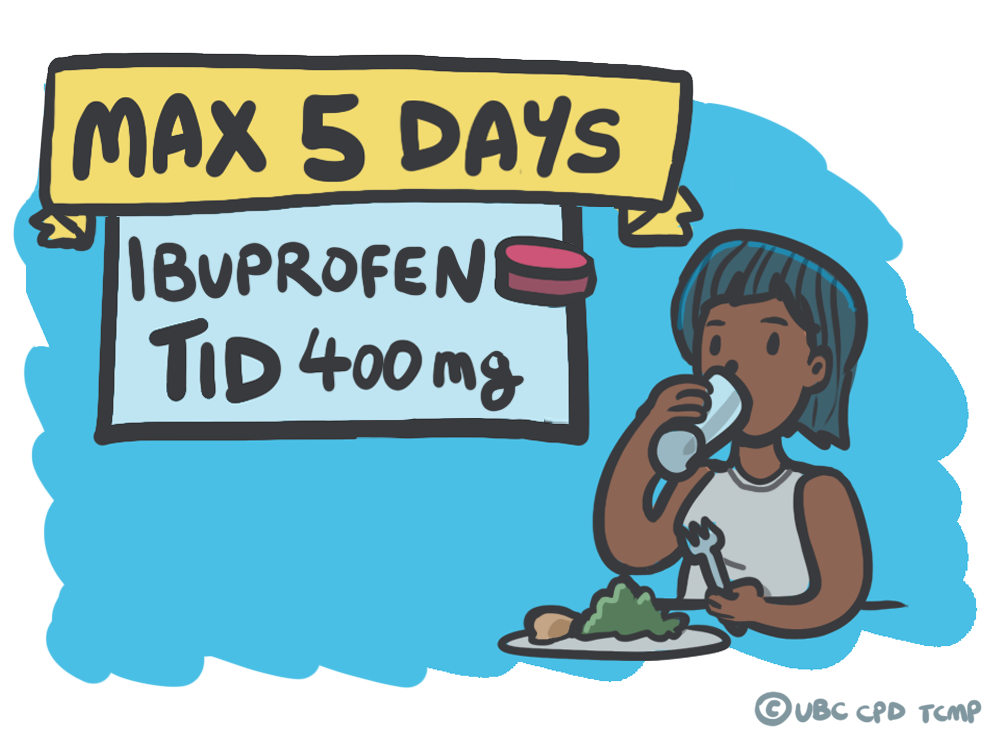
Other NSAIDs (ibuprofen, naproxen, diclofenac) do not have the same FDA warning or data strictly limiting duration. However, it is the authors’ belief that patient-specific factors, including bleeding risk, should be incorporated into treatment plans with pain reassessment after 5 days. This is supported by several studies measuring the analgesic benefits of NSAIDs. The duration of evidence typically ranges between 2-5 days before reassessment for acute pain.16, 17, 18
What I do now
Based on the above evidence, I now appreciate the increased risk-to-benefit ratio that exists when dosing ibuprofen and ketorolac above the known analgesic ceiling doses. I currently incorporate this ‘NSAID ceiling’ into my prescribing practice for anti-inflammatory medications. Accounting for patient factors, co-ingested and prescribed substances, I typically prescribe maximum individual doses of 400 mg oral ibuprofen and 10 mg intramuscular ketorolac. I counsel my patients where possible to limit their NSAID use to a 5-day window and encourage other non-pharmacological and multimodal analgesia when educating them about the ceiling doses. I provide thrice daily maximum oral dosing ‘only with meals’ recommendations to my patients when prescribing these NSAIDs and suggest reassessment at five days.
References
- Guidelines and Protocols Advisory Committee (GPAC). BCGuidelines.ca: Managing Patients with Pain in Primary Care – Part 2 (2022). Government of British Columbia. Effective Date: February 23, 2022. Accessed Feb 10, 2023. (View)
- Harris RC, Breyer MD. Update on cyclooxygenase-2 inhibitors. Clin J Am Soc Nephrol. 2006;1(2):236-245. doi:10.2215/CJN.00890805 (Request with CPSBC or view with UBC)
- Brunton LL Knollmann Björn C. Goodman & Gilman’s the Pharmacological Basis of Therapeutics. Fourteenth ed. New York: McGraw Hill; 2023. (View with CPSBC or UBC)
- Motov S, Masoudi A, Drapkin J, et al. Comparison of Oral Ibuprofen at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2019;74(4):530-537. doi:10.1016/j.annemergmed.2019.05.037 (View with CPSBC or UBC)
- Ong CK, Lirk P, Tan CH, Seymour RA. An evidence-based update on nonsteroidal anti-inflammatory drugs. Clin Med Res. 2007;5(1):19-34. doi:10.3121/cmr.2007.698 (View)
- Motov S, Yasavolian M, Likourezos A, et al. Comparison of Intravenous Ketorolac at Three Single-Dose Regimens for Treating Acute Pain in the Emergency Department: A Randomized Controlled Trial. Ann Emerg Med. 2017;70(2):177-184. doi:10.1016/j.annemergmed.2016.10.014 (View with CPSBC or UBC)
- Staquet MJ. A double-blind study with placebo control of intramuscular ketorolac tromethamine in the treatment of cancer pain. J Clin Pharmacol. 1989;29(11):1031-1036. doi:10.1002/j.1552-4604.1989.tb03274.x (Request with CPSBC or view with UBC)
- Peirce RJ, Fragen RJ, Pemberton DM. Intravenous ketorolac tromethamine versus morphine sulfate in the treatment of immediate postoperative pain. Pharmacotherapy. 1990;10(6 ( Pt 2)):111S-115S. (Request from CPSBC or from UBC)
- Brown CR, Moodie JE, Wild VM, Bynum LJ. Comparison of intravenous ketorolac tromethamine and morphine sulfate in the treatment of postoperative pain. Pharmacotherapy. 1990;10(6 ( Pt 2)):116S-121S. (Request from CPSBC or from UBC)
- Reuben SS, Connelly NR, Lurie S, Klatt M, Gibson CS. Dose-response of ketorolac as an adjunct to patient-controlled analgesia morphine in patients after spinal fusion surgery. Anesth Analg. 1998;87(1):98-102. doi:10.1097/00000539-199807000-00021 (View with CPSBC or UBC)
- Minotti V, Betti M, Ciccarese G, Fumi G, Tonato M, Del Favero A. A double-blind study comparing two single-dose regimens of ketorolac with diclofenac in pain due to cancer. Pharmacotherapy. 1998;18(3):504-508. (Request with CPSBC or view with UBC)
- García Rodríguez LA, Cattaruzzi C, Troncon MG, Agostinis L. Risk of hospitalization for upper gastrointestinal tract bleeding associated with ketorolac, other nonsteroidal anti-inflammatory drugs, calcium antagonists, and other antihypertensive drugs. Arch Intern Med. 1998;158(1):33-39. doi:10.1001/archinte.158.1.33 (Request with CPSBC or view with UBC)
- Strom BL, Berlin JA, Kinman JL, et al. Parenteral ketorolac and risk of gastrointestinal and operative site bleeding. A postmarketing surveillance study. JAMA. 1996;275(5):376-382. doi:10.1001/jama.1996.03530290046036 (Request with CPSBC or view with UBC)
- Traversa G, Walker AM, Ippolito FM, et al. Gastroduodenal toxicity of different nonsteroidal antiinflammatory drugs. Epidemiology. 1995;6(1):49-54. doi:10.1097/00001648-199501000-00010 (Request with CPSBC or view with UBC)
- Menniti-Ippolito F, Maggini M, Raschetti R, Da Cas R, Traversa G, Walker AM. Ketorolac use in outpatients and gastrointestinal hospitalization: a comparison with other non-steroidal anti-inflammatory drugs in Italy. Eur J Clin Pharmacol. 1998;54(5):393-397. doi:10.1007/s002280050481 (Request with CPSBC or view with UBC)
- Riff DS, Duckor S, Gottlieb I, et al. Diclofenac potassium liquid-filled soft gelatin capsules in the management of patients with postbunionectomy pain: a Phase III, multicenter, randomized, double-blind, placebo-controlled study conducted over 5 days. Clin Ther. 2009;31(10):2072-2085. doi:10.1016/j.clinthera.2009.09.011 (View with CPSBC or UBC)
- Gibofsky A, Silberstein S, Argoff C, Daniels S, Jensen S, Young CL. Lower-dose diclofenac submicron particle capsules provide early and sustained acute patient pain relief in a phase 3 study. Postgrad Med. 2013;125(5):130-138. doi:10.3810/pgm.2013.09.2693 (Request with CPSBC or view with UBC)
- Altman R, Daniels S, Young CL. Indomethacin submicron particle capsules provide effective pain relief in patients with acute pain: a phase 3 study. Phys Sportsmed. 2013;41(4):7-15. doi:10.3810/psm.2013.11.2031 (Request with CPSBC or view with UBC)

What about anti inflammatory effects? Is that different than the analgesic effect? Or was it not measured?
Do you add other analgesics in case you can not manage patient’s pain?
What is the rationale for advising taking NSAIDs with food? Do they act as local irritants and thus will increase the bleeding risk? Isn’t the bleeding risk from the enzymatic effects? Food just delays absorption.
What about individuals taking multiple analgesics to manage their chronic pain?
I appreciate the information Dr Varshney dwelled upon and explained. My question is: were weight, gender, race, co-morbidities & other medications the trial population was taking during study time etc. considered and included during the study?
I am aware of te risk associated with NSAIDs and the difference between COX 1 and 2. But the surprising information is that it took only 5 days to see the harm.
In elderly patients one is often stuck with Acetominophen and opioids only, due to concerns about their kidneys. Opioids in elderly are also not ideal. Are there any alternatives to NSAIDS and opioids in the elderly? In an 80 year old with normal kidney function is it save to administer NSAIDs for a few days. Are we going to see iv Acetominophen in Canada?
Motov’s study compares IV ketoralac doses, not IM doses as you’ve mentioned. Are you inferring that the IM and IV doses have similar efficacy for ketoralac?