By Hans Haag and Dr. Ricky Turgeon on July 5, 2023
Heart failure is the third leading cause of hospitalization in Canada and leads to readmission in 1 in 5 patients within 30 days after discharge. Iron deficiency (with or without anemia) is an important comorbidity in patients with HF and is associated with worse outcomes. Assess iron deficiency for all patients with HFrEF and HFmrEF admitted for acute HF.
By Dr. Michael Diamant on April 19, 2022
The prevalence of ambulatory patients with advanced or end-stage heart failure (HF) is increasing over time, and now comprises as much as 14% of all patients with HF. Patients may be eligible for advanced therapies, including durable mechanical circulatory support (MCS) and heart transplantation, that can change their trajectory and markedly improve long-term survival.
By Shari Hurst on April 6, 2022
There are a few tips and tricks to improve medication tolerance and adherence, and improve quality of life for patients with HF-rEF. Multiple studies have shown that a focus on patient education and empowerment along with clinical follow-up for HFrEF medical treatment improves survival, reduces hospitalizations, and improves quality of life.
By Drs. Christopher Cheung, Kenneth Gin, Jason Andrade on February 10, 2021
Patients with persistent AF, less symptomatic and/or older patients, and those with prior anti-arrhythmic failure are best managed with a rate control strategy. The EAST-AFNET 4 study is a practice-changing trial, and strongly supports the role of early rhythm control in patients with newly-diagnosed AF.
By Tanveer Brar BSc BSc(Pharm) ACPR, Doson Chua BSc(Pharm) PharmD FCSHP BCPS BCCP, and Laura Atiyeh on January 13, 2021
Heart failure (HF) is a clinical syndrome associated with significant morbidity and mortality. In 2020, the prevalence of HF was approximately 64.34 million cases (8.52 per 1,000 inhabitants) worldwide and this number has been steadily increasing over time. There is compelling evidence to suggest that in individuals with HFrEF in the presence or absence of T2DM, both dapagliflozin and empagliflozin have profound effects on reduction of HF hospitalizations and possibly CV mortality.
By Omid Kiamanesh, MD, FRCPC on August 26, 2020
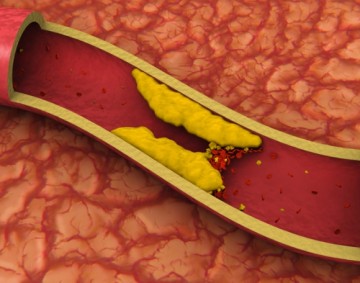
Despite intensive lowering of LDL-C using lipid-modifying therapy, residual ASCVD risk persists, particularly in those with hypertriglyceridemia. Icosapent ethyl has been shown to reduce residual ASCVD risk and cardiovascular death in select patients with hypertriglyceridemia while on statin therapy.
By Drs. Nima Moghaddam, Christopher Cheung, Kenneth Gin on July 15, 2020
The debate over the optimal management in stable ischemic heart disease has grown over the past decade with more evidence supporting a conservative medical therapy approach over an upfront invasive strategy with coronary revascularization. However, there remains significant practice variation in deciding when to pursue coronary revascularization.
By Dr. Alice S Chang, Dr. Michael J Diamant, Dr. Margot K Davis, and Dr. Krishnan Ramanathan on October 30, 2019
Cardiac amyloidosis (CA) is an infiltrative disease that is being increasingly identified in those with HFpEF. Amyloidosis is a group of heterogeneous disorders characterized by the deposition of misfolded protein that aggregates into fibrils, affecting multiple organs including the heart, neural tissues, kidneys, and the gastrointestinal tract.
By Drs. Terence Yung and Steve Ham on December 5, 2018
All postoperative troponin elevation should be treated seriously. Troponin elevation after surgery is associated with significant mortality at 30 days. Myocardial injury after non-cardiac surgery (MINS) diagnosis is made after other causes of troponin elevation are ruled out. Up to 90% of patients with a troponin elevation postoperatively do not exhibit any symptoms, yet their outcomes are still poor.
By Drs. Terence Yung and Tony Wan on July 24, 2018
For those who had an elective hip or knee arthroplasty who have no other risk factors for VTE, after initial 5 days of DVT prophylaxis with rivaroxaban 10mg a day, I complete the remaining DVT prophylaxis with aspirin 81mg once daily for an additional 30 days for hip arthroplasty and 9 days for knee arthroplasty. Those who already were on once-daily 81mg aspirin prior to surgery will receive 162mg aspirin once daily instead in this period.
By Doson Chua, PharmD, FCSHP, BCPS(AQ) and Dr. Mustafa Toma on January 10, 2018
Sacubitril/valsartan is the first in class of ARNI and has proven its superiority in reducing mortality and morbidity in HFrEF as compared to the use of ACEI. Sacubitril/valsartan should be considered in patients who are symptomatic despite optimal or maximally tolerated guideline-driven HF therapies consisting of a beta blocker, ACEI/ARB and MRA. Monitoring of patients on sacubitril/valsartan is similar to ACEI.
By Drs. Christopher Cheung and Kenneth Gin on August 9, 2017
Perioperative management of anticoagulation is challenging as physicians must consider the risks of stroke, systemic embolism, and perioperative bleeding.
By Dr. Gordon Francis on April 26, 2017
High Lp(a) is a major CVD risk factor that should be measured and acted upon in patients and families where there is history of premature CV events but lack of clear risk factors, and in patients with known CVD and recurrent events despite treatment to LDL-C target.
By Drs. Terence Yung and Erin Morley on March 22, 2017
Physicians who see patients for preoperative assessment often face the dilemma of accurately determining a patients’ cardiac risk. Patients may have limited mobility and thus do not necessarily elicit cardiac symptoms even if there is significant flow-limiting coronary artery disease.
By Drs. Christopher Cheung and Kenneth Gin on June 22, 2016
Hypertension affects over 1 in 5 Canadians and is one of the leading causes of cardiovascular disease, including coronary artery disease and heart failure. Uncontrolled hypertension is a risk factor for stroke (both ischemic and hemorrhagic), retinopathy, chronic kidney disease (CKD), and peripheral vascular disease. Epidemiologic studies show that the risk of cardiovascular disease increases above a blood pressure of 115/75 mmHg.
By Dr. Daniel Kim on February 3, 2016
Supraventricular tachycardia (SVT) is a dysrhythmia characterized by abrupt onset, regular rate that usually exceeds 150 beats/minute, and lack of identifiable P waves on ECG. SVT is caused by an abnormal circuit that allows a wave of depolarization to repeatedly travel in circular fashion in cardiac tissue via a reentry circuit that may reside in the atrioventricular (AV) node or outside the AV node in an accessory pathway.
By James McCormack on September 16, 2015
Numerous observational studies have consistently shown in many (but not all) patient populations a correlation between people with higher blood pressure, glucose, and cholesterol numbers, and a greater risk of cardiovascular events such as heart attacks, strokes, and other unwanted outcomes.
By Dr. Mustafa Toma and Dr. Christopher Cheung on May 27, 2015
There are approximately 500,000 Canadians living with heart failure, and more than 10% in patients older than 65. Up to 50% of patients presenting with signs and symptoms of heart failure will have a preserved ejection fraction (HFpEF or diastolic dysfunction). However, there is a lack of evidence for effective therapies in the management of HFpEF.
By Dr. Mustafa Toma and Dr. Christopher Cheung on October 15, 2014
In patients presenting with acute decompensated heart failure and previously on oral loop diuretics at home, there is no difference between low-dose and high-dose furosemide, or bolus and continuous infusions, on the patient’s global assessment of symptoms and changes in serum creatinine at 72 hours.
By Dr. Nadia Zalunardo on September 15, 2014
The most common cause of death among individuals with chronic kidney disease is cardiovascular disease. For most people with CKD, the risk of cardiovascular death exceeds the risk of developing end stage kidney disease.
By Dr. Tara Sedlak on April 14, 2014
Women with myocardial infarction (MI) have a two fold higher rate of no obstructive coronary artery disease (CAD), defined as <50% stenosis in any epicardial coronary artery on angiogram, than men. Despite this, outcomes including death during hospitalization following an MI are higher among women (particularly women <55 years) as compared to men.
By Dr. Natasha Press on March 5, 2014
The most recent AHA guidelines (2007) have limited antibiotic prophylaxis to those patients at highest-risk for developing endocarditis and who are undergoing high-risk invasive procedures.
By Drs. Kam Shojania and Neda Amiri on September 23, 2013
Rheumatoid arthritis has been described to be associated with an increased risk of cardiovascular disease. This risk appears to be multifactorial in nature. However, there is emerging evidence that glucocorticoids play a role.
By Drs. Mustafa Toma and Neda Amiri on April 15, 2013
Spironolactone or eplerenone should be added to BB and ACEi/ARB in NYHA class II HF patients with EF < 30-35% in the absence of significant renal impairment or hyperkalemia.
By Dr. Jiri Frohlich on August 20, 2012
Several studies established that apo B is a better predictor of risk both at baseline and on treatment than LDL-C due to the fact that small dense LDL particles are much more atherogenic as they easily penetrate the endothelial space.
By Dr. Steve Wong on November 2, 2010
I now strongly consider using dabigatran instead of warfarin in patients with a CHADS score of 2 or higher.
By Dr. Steve Wong on April 20, 2010
I generally started with thiazide diuretics (due to cost and proven effectiveness) then added either an ACE inhibitor (ACEi) or a calcium channel blocker (CCB), consistent with the Canadian Hypertension Society Guidelines.
By Dr. Breay Paty on April 15, 2010
Since their introduction, certain contraindications and side effects have been well known, including worsening heart failure, edema (including macular edema) and weight gain.












Recent Comments