By Dr. Kelvin Lou & Dr. David M. Williscroft on June 25, 2025
Discussing code status is a critical part of the larger goals of care discussion, but code status discussions often happen in emotional and high-stake situations. Directly addressing the high levels of emotion in these situations can greatly enhance communication and decision making. The focus of this approach is on building a personal connection and fostering trust at each step. To address the time limitations in acute care, we have streamlined multiple communication tools into the acronym HEEART, and provided tips on word choice and helpful practices.
By Dr. Ilona Hale on April 23, 2025
Until recently, I had never really considered that testing and treatments have an environmental cost. The burden of overuse is not trivial: up to 30% of all tests and treatments we order are unnecessary and an additional 10% are harmful to our patients. I have realized that if I really want to make a difference to my carbon footprint at work, reducing unnecessary care has a greater impact than recycling clinic waste or powering down my computer.
By Dr. Heather Fulton on November 26, 2024
I recommend Community Reinforcement and Family Training (CRAFT) for families who have a loved one with substance use challenges. It is a is a science-backed approach that helps family members change the way they interact with their loved one that makes change more likely while also helping themselves in the process.
By Dr. Michelle C. Chan on October 22, 2024
Recent studies on options in family planning have changed my practice, and I now routinely take the opportunity when reviewing family planning options for people who are at risk of becoming pregnant and do not want to be pregnant to review emergency contraception and abortion as options in family planning.
By Dr. Ilona Hale on September 16, 2024
For many years, I failed to recognize the unique potential I had to make a difference to the environment as a clinician, from within my own practice. However, using a planetary health approach in clinical practice not only allows us to reduce environmental impacts but also offers many co-benefits: better health outcomes, lower costs, decreased workload, and a more resilient and sustainable system.
By Dr. Sarah McCorquodale on June 17, 2024
Having evidence that remission of type 2 diabetes is possible through weight loss in select people, I have changed my approach to prevention and management of type 2 diabetes.
By Dr. Rohit Vijh on May 21, 2024
Given the increasing rates of syphilis and changing epidemiology of syphilis with increasing incidence in heterosexual populations, my clinical suspicion for syphilis testing has increased. If a patient presents with primary or secondary lesions that are amenable to PCR swabbing, I now collect a PCR swab specimen, in addition to sending the patient for serology.
By Dr. Omesh Syal on April 15, 2024
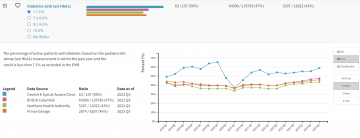
I highly recommend registering with the Health Data Coalition and becoming more familiar with your measures within the HDC Discover application to recognize your contribution. We, as a collective profession, can make a positive impact on our own practices and larger communities.
By Dr. Paxton Bach on March 12, 2024
The new Canadian guideline situates alcohol-related harms along a continuum, recognizing that negative health and social consequences of alcohol can arise even at rates previously consistent with low risk.
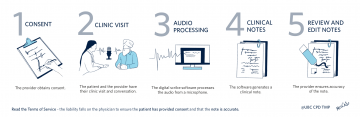
By Rohit Singla PhD, Dr. Daniel Raff, Dr. Hester Vivier, and Dr. Andre Van Wyk on February 14, 2024
Conversational AI has become a valuable tool for family physicians in Canada. It helps us provide better patient care, eases the burden of documentation, and reduces burnout. Incorporating digital scribe technology brings marked efficiency, especially given the high patient volumes. With AI managing real-time transcription and summarization, physicians can give undivided attention to patients, deepening rapport and focus on prescriptions and referrals.
By Drs. Kevin Liang and Philip Hui on January 10, 2024
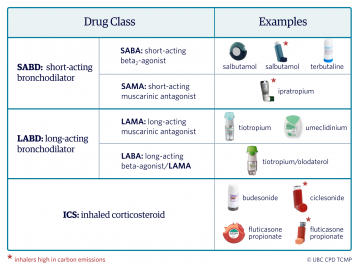
New asthma and COPD guidelines are changing the way we provide respiratory care; SABDs, such as salbutamol and ipratropium, are no longer the mainstay treatment for both conditions. Importantly, SABD overuse is a measure of poor disease control and suggests a need for treatment escalation.
By Dr. Shirley Samuel-Haynes on November 21, 2023
I learned that a palliative approach to care and serious illness conversations address and manage patients’ and families’ psychological, practical, social, loss/grief, spiritual, and physical issues like pain and symptom management in line with their goals of care and help prepare for eventual life closure. Here are practical tips on how to implement this in your practice.
By Dr. Rachel Grimminck, Dr. Jo Hoffman, and Dr. Laura McLean on October 25, 2023
Given the rapidly shifting social, political, and legal contexts surrounding the use of psychedelics, we realized the need to offer an informed opinion on the use of psychedelics in the same way we offer information and harm reduction strategies for substances such as opiates, cannabis, and alcohol.
By Drs. Jill Norris and Jessica Otte on September 12, 2023
Primary care clinicians face an overwhelming volume of information to process and tasks to complete. There are new and sometimes conflicting guidelines and practice standards, forms to fill out, emails about meetings, and an inbox full of labs, documents to review, and messages to respond to. Now that I get Portraits in my email inbox from time to time, I schedule time to look at them, and focus on the listed recommendations and whether my pattern of practice is close to where it should be according to the evidence, and if not, why not.
By Drs. Domnick Manhas and Tony Wan on August 23, 2023
It is estimated that 15% of all cancer patients will develop VTE, resulting in significant morbidity and mortality. The cost of cancer-associated thrombosis is substantial to the healthcare system. Currently, routine thromboprophylaxis is not recommended given the fear of increased risk of bleeding, modest absolute risk reduction in VTE, and inconvenience. However, a selected group of cancer patients with very high VTE risk will benefit from thromboprophylaxis.
By Jamison Falk, PharmD on June 19, 2023
While I’ve been hard on newer medications like SGLT2i for their relatively small benefit in lower-risk patients, recent systematic reviews show that our traditional interventions are no better, and may be worse, at reducing risks of outcomes. I now discuss the option of adding an SGLT2i with patients with diabetes and pre-existing cardiovascular or renal disease or with symptomatic hyperglycemia where blood glucose reduction would be expected to reduce day-to-day symptoms. I reduce or discontinue doses of other antihyperglycemic medications if possible when starting an SGLT2i and I educate patients about potential adverse events.
By Dr. Emma Coffey on April 3, 2023
Many patients don’t know that an IUD is a highly effective option for emergency contraception. We can offer patients either the 52mg LNG-IUS (up to 5 days) or the copper IUD (up to 7 days) for EC. Both options are highly effective at preventing pregnancy (>99%).
By Drs. Clara Lu and Renée Janssen on March 7, 2023
Since the publication of the 2020 ATS Clinical Practice Guideline on pharmacologic treatment in tobacco-dependent adults, I now explain the goals of pharmacotherapy for tobacco use disorder in terms of reducing the compulsion to smoke and increasing readiness to quit, rather than abstinence alone. If patients are open to the conversation, I will discuss and offer all pharmacotherapy options — but emphasize the efficacy and safety of varenicline as my preferred first-line agent.
By Drs. Jennifer Kask and Kirsten Duckitt on January 25, 2023
Preterm birth is the leading cause of perinatal morbidity and mortality in British Columbia and worldwide. We now carefully elicit any history of previous preterm birth and offer vaginal progesterone therapy for ANY history of spontaneous preterm birth. We fill in the Special Authority Request and give out the patient handout even before the patient goes to the pharmacy. We also encourage women to continue the medications until 37 weeks of gestational age.
By Dr. Caitlin Dunne on November 30, 2022
Polycystic ovary syndrome is the most common endocrinopathy in women of reproductive age. It affects 8%–13% of young women and its symptoms are some of the most prevalent concerns that community physicians encounter. In many cases, diagnosis and management can be carried out in a virtual health setting using clinical criteria and judicious use of laboratory investigations.
By Drs. Piszczek, Wright, and Grant on November 16, 2022
My approach now is to have the confidence to reassure patients who are low risk that SARS-CoV2 infection will most likely be mild for them and that no specific therapy is needed. Those who are of intermediate risk will also generally do well, but it is an opportunity to create a plan of what to do if they have flu-like symptoms, including their preferences should they test COVID positive. For those who are at high risk, especially CEV-1, I ensure them that there is a clear testing and treatment plan. Any physician can prescribe Nirmatrelvir/rt. A step-by-step instruction guide for prescribing is available on the BCCDC website.
By Drs. Fiona Petigara and Joanna Cheek on September 28, 2022
A large part of physician’s day is spent on mental health and wait times to see specialists can be very long. In 2022 the BC Government created “Group Medical Visit” (GMV) codes to promote physicians to deliver services to groups of patients as “an effective way of leveraging existing resources; simultaneously improving quality of care and health outcomes, increasing patient access to care and reducing costs” (BC Gov, 2022). Physicians can now refer their patients to the Group Cognitive Behavioral Therapy program via cbtskills.ca or through PathwaysBC fillable PDF and they can also train to facilitate group medical visits.
By Dr. Katarina Wind on May 3, 2022
Medical school taught me that “obesity” is a cause of morbidity and mortality, and that weight loss is its cure. I recorded patients’ BMIs and counselled them on weight-loss strategies, believing that I was helping them.
By Brendan McNeely and Dr. Amanda Hu on February 9, 2022
Recent evidence has emerged that shows cannabis smoking is related to significant patient morbidity. Namely, cannabis smoke exposure increased the risk of oropharyngeal cancer in a dose-dependent manner. Cannabis use may also be associated with hearing loss, vestibular dysfunction, tinnitus, and sinusitis.
By Drs. Taylor Drury, Poupak Rahmani, and Tony Wan on January 26, 2022
We continue to use full dose therapeutic low molecular weight heparin (LMWH) for bridging in the pre-operative period. However, we now use post-operative prophylactic LMWH as an alternative bridging strategy in patients undergoing high-risk bleeding procedures. In patients at high risk of thromboembolism (including mechanical mitral valve and atrial fibrillation) undergoing a high-risk bleeding procedure, we are now less aggressive in resuming full dose therapeutic anticoagulation, as we feel comfortable using prophylactic LMWH for up to several days post-operatively before resuming therapeutic anticoagulation.
By Gerri Klein on January 12, 2022
For all my patients who are on hypoglycemic medications, oral or injectable, I suggest using rtCGM or isCGM. Even intermittent use or a short trial of 10 days to two weeks with either of these devices can be enlightening for patients. With the ongoing COVID restrictions, many of my patients have been unable (or unwilling) to obtain an A1C from a lab test. In my practice, I have found it helpful to use glucose TIR to assess glucose control as an adjunct measure to A1C results; when an A1C is not available; and to guide treatment recommendations.
By Dr. Linda Uyeda and Dr. Ashley Miller on July 7, 2021
The ingredients needed to create a happy workplace also largely reflect the principles of secure attachment. Across all levels within organizations, if people do not feel “safe, seen, soothed, and secure” they are more likely to make errors, breach safety protocols, and struggle working together as a team.
By Sue Barlow and Carolyn Rondeau on June 3, 2021
Concussions or mild traumatic brain injury are the most common type of traumatic brain injury. It is estimated that every year in British Columbia (BC), there are approximately 14,500 visits to the emergency department and that this number is most likely an underestimate of the “true burden of concussion”.
By Dr. Ashley Miller and Dr. Linda Uyeda on May 12, 2021
As I started to understand that this pandemic would wear on, I had to figure out how to help my patients’ families and my own family navigate our way through this totally new reality. I drew on the science of attachment, resilience and healthy relationships to make a plan. (Please stay tuned for Article #3!)












Recent Comments