By Dr. Leslie Sadownik on February 13, 2019
Lichen sclerosus (LS) is a chronic skin disorder with a remitting and relapsing clinical course. Women commonly present with severe vulvar itch and an urge to scratch the skin. The recommended treatment is a course of topical steroids. Most women will improve with treatment. However, some will report, “the steroids did not help”. Here are some practice tips to help.
By Drs. Maysam Khalfan and Kam Shojania on January 30, 2019
Patients who present with non-specific symptoms are sometimes tested with rheumatologic lab investigations as part of a ‘panel’ of tests. When these tests come back positive, it can lead to more confusion, patient anxiety, misdiagnosis or unnecessary referral.
By Andrea Holmes on January 16, 2019
Breast and prostate cancer survivors want to know what to eat to prevent cancer from coming back. HealthLink BC healthy eating resources that support successful dietary and physical activity change for prostate and breast cancer survivors are available for your patients.
By Mark W. Hull MD MHSc on November 13, 2018
Over the last five years, on an ongoing basis, we have seen new HIV infections occurring in young gay, bisexual and other men who have sex with men (MSM). The majority of these individuals had had a prior negative HIV test within the last year, or were presenting with signs or symptoms supportive of an acute HIV infection, suggesting recent exposure and transmission of HIV infection, highlighting the need for novel HIV prevention strategies.
By Dr. Diane Villanyi on October 31, 2018
Under Section 230 of the Motor Vehicle Act, in addition to physicians, registered psychologists, optometrists and nurse practitioners are obliged to report a patient who may be unfit to drive. RoadSafetyBC has a dedicated phone line for medical professionals to help with complex cases.
By Michelle C. Danda, RN, BN on October 10, 2018
I realized that engagement is paramount when working with an ambivalent patient, because the change that they want to make is often important in their life, even if the clinician views it as a problem behavior. Motivational interviewing education has been shown to improve patient alliance and treatment adherence.
By Dr. Martha Spencer on September 19, 2018
Fecal incontinence (FI), defined as the involuntary passage of stool or the inability to control the expulsion of stool, is a common but under-reported condition that can affect people of all ages but has increased prevalence in older adults.
By Dr. Carol-Ann Saari on September 5, 2018
In the general population, approximately 75% of Canadians will report having experienced an adverse and potentially traumatic experience in their lifetime, with 9.2% meeting criteria for PTSD. We have to become trauma informed. Trauma informed practice (TIP) is a way of providing services that recognizes the need for physical and emotional safety, choice and control in decisions affecting one’s treatment and an environment where patients do not experience further traumatization.
By Dr. Colleen Varcoe and Dr. Heather Smith on August 15, 2018
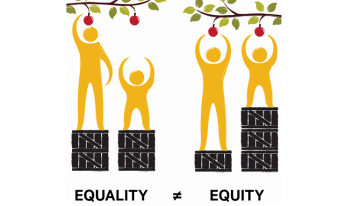
Health equity-oriented care is now part of my daily practice; the tools created with, and provided by, the EQUIP study have helped to make health care inequity an issue that I can screen for and offer options for management.
By Dr. Maia Love on July 4, 2018
Defining yourself as a person first, and your role as a professional second, has benefits in preventing burnout and creating more personal energy. Put your own oxygen mask on first.
By Dr. Min S. Phang, MRCP, FRCPC and Stacey Miller, PT on June 13, 2018
I now refer all children with cerebral palsy, or suspected cerebral palsy, to the Child Health BC Hip Surveillance Program. Information about the program is available at www.childhealthbc.ca/hips, including a referral form for physicians. The incidence of hip dislocations can be significantly reduced!
By Dr. Kelly Luu on May 23, 2018
Evidence shows that the strategy which physicians frequently employ, educating and training, is only the first step in the process of behavioural change. By helping patients shift their narratives about themselves, we can strengthen their ability to have sustained behavioural change.
By Dr. Andrew Howard, Tyler Schwaiger, Dr. Noah Silverberg, and Dr. Will Panenka on May 2, 2018
Rest might increase symptoms and recovery time following concussion or mild traumatic brain injury. Inactivity has been associated with physical deconditioning, social isolation, discouragement about recovery, and reactive anxiety and depression. Early mobilization and graded exercise programs can reduce post-concussive symptoms and recovery time.
By Dr. Vanessa Brcic and Dr. Devon Christie on April 18, 2018
What changed our practice was a fundamental recognition of trauma as a determinant of health, and furthermore, that PTSD is only the tip of the iceberg when it comes to trauma. Much lies under the surface for our patients.
By Dr. Leslie Sadownik on April 4, 2018
Women with chronic vulvar disorders will often report years of symptoms before an accurate diagnosis is made, and effective treatment is started.
By Dr. Laura Sauvé on February 7, 2018
Vaccines are safe, but sometimes adverse events following immunizations do happen, and can be very concerning to families. If your patient has an AEFI, there is a voluntary reporting system. Public Health Officers in your local Health Authority will be able to answer most questions or concerns.
By Ruth Elwood Martin on January 23, 2018
To address the issue of health care discrimination and coordination of care people with incarceration history, the CCPHE has collaboratively developed Guidelines for Family Physicians working with Formerly Incarcerated People.
By By Dr. Christy Sutherland and Emily Wagner on November 15, 2017
I no longer offer rapid methadone tapers to my patients. Buprenorphine/naloxone is now recommended as the first-line opioid agonist treatment for opioid use disorder in British Columbia. This is because of its superior safety profile when compared with methadone as well as an easier transition to take home dosing.
By Dr. Roberto Leon on November 1, 2017
I came across a publication in the British Medical Journal by Sarah A. Schoeman: Assessment of best single sample for finding chlamydia in women with and without symptoms: a diagnostic test study. Participants took a vaginal swab before a routine gynecological exam, and clinicians then took an endocervical swab during examination.
By Dr. Jennifer Robinson on October 18, 2017
MOVE an injury: Movement, not rest. Options: offer other options for cross training. Vary rehabilitation with strength, balance and agility drills. Ease back to activity early for emotional strength.
By Dr. Eileen Murray on October 3, 2017
When I started out in dermatology, corticosteroids were the only systemic drug available to treat patients with severe allergic contact dermatitis (ACD), atopic dermatitis (AD), drug reactions and those with bullous diseases. Corticosteroids are potent and excellent immunosuppressive agents. The main problem with systemic use is the high risk of drug interactions, as well as multiple serious acute and long-term side effects.
By Dr. Taryl Felhaber on September 20, 2017
Why should physicians encourage early and ultimate return to work whenever they can? In a nutshell, because it is usually in the patient’s best interest to remain in the workforce.
By Drs. Christopher Cheung and Kenneth Gin on August 9, 2017
Perioperative management of anticoagulation is challenging as physicians must consider the risks of stroke, systemic embolism, and perioperative bleeding.
By Dr. Anne Antrim on July 18, 2017
The current definition of Autism Spectrum Disorder has 2 criteria: “persistent impairment in reciprocal social communication and social interactions” AND “restricted, repetitive patterns of behavior”. The symptoms must be present from early childhood, but may not manifest till the social demands exceed the capacity of the child to respond.
By Dr. Roberto Leon on June 20, 2017
One of the most complex decisions that women (and their physicians) occasionally need to take in mid-life is whether to use prescription medications for their menopausal symptoms. Previously known as Hormone Replacement Therapy (HRT), Menopause Hormone Therapy (MHT) is an effective and evidence based treatment for moderate to severe hot flashes and/or night sweats (defined as bothersome enough to interfere with daily activities, impair quality of life and/or interrupt sleep).
By Cait O'Sullivan on May 31, 2017
When I identify strong drug therapy recommendations of particular relevance to my practice scope, I seek collateral information and there are two resources I routinely incorporate into my literature search. I start with the Cochrane Library and then check to see whether a FDA advisory committee has weighed in on key issues.
By Dr. Randall White on May 10, 2017
When psychiatric patients are treated in an emergency department, they are often hypervigilant, manic, or otherwise in an excited, agitated state. The current standard of care to manage acute agitation in adults is using an antipsychotic medication and a benzodiazepine, often loxapine or haloperidol and lorazepam.
By Drs. Charlie Chen and Hayden Rubensohn on April 12, 2017
What is the patient willing to consent to as treatment if his/her condition were to seriously deteriorate? The Serious Illness Conversation Guide developed by Ariadne Labs provides a framework for physicians to engage in care planning with patients in a manner acceptable to the patient.
By Dr. Dan Bilsker on March 8, 2017
Treatment plan should specifically target psychological problems that are barriers to occupational, relationship or emotional function, rather than broadly defined issues. Being able to return to work is a substantial benefit for the individual: staying at home for an extended time is damaging to the individual’s self-esteem, coping ability and psychological health. Practice “positive psychology”, emphasizing the outcomes that determine the meaning and success of one’s life and focus on individual’s strengths to reach goals.
By Dr. Martha Spencer on February 22, 2017
Martha Spencer, MD, FRCPC, Providence Health Care, Clinical Instructor, UBC (biography and disclosures) Disclosures: Education grant from Pfizer to help support my incontinence fellowship in Edmonton, Grant from Pfizer ($10 000) to support start-up costs for the Geriatric Continence Clinic at SPH. Mitigating potential bias: Only published trial data is presented and recommendations are consistent […]


























Recent Comments