By Dr. Rachel Grimminck, Dr. Jo Hoffman, and Dr. Laura McLean on October 25, 2023
Given the rapidly shifting social, political, and legal contexts surrounding the use of psychedelics, we realized the need to offer an informed opinion on the use of psychedelics in the same way we offer information and harm reduction strategies for substances such as opiates, cannabis, and alcohol.
By Vinicio Delgado and Dr. Wayne Lai on July 19, 2023
Insomnia is one of the most commonly reported sleep disorders at our sleep clinic. Despite its prevalence, treating it can be challenging due to its complex and multifactorial nature. A comprehensive and personalized approach to treatment is, therefore, necessary for effective management. However, providing this level of support requires significant time and resources. Offering a self-help intervention as a complement to care can help reach patients who might not otherwise receive CBTi or refuse onsite treatment.
By Dr. Elisabeth Baerg Hall on October 19, 2022
October is ADHD Awareness Month. Until recently, female presentations of ADHD have been largely overlooked in both clinical and research settings. With increasing awareness and media attention to women and ADHD, adult women are asking if ADHD could explain their longstanding challenges.
By Drs. Fiona Petigara and Joanna Cheek on September 28, 2022
A large part of physician’s day is spent on mental health and wait times to see specialists can be very long. In 2022 the BC Government created “Group Medical Visit” (GMV) codes to promote physicians to deliver services to groups of patients as “an effective way of leveraging existing resources; simultaneously improving quality of care and health outcomes, increasing patient access to care and reducing costs” (BC Gov, 2022). Physicians can now refer their patients to the Group Cognitive Behavioral Therapy program via cbtskills.ca or through PathwaysBC fillable PDF and they can also train to facilitate group medical visits.
By Dr. Elisabeth Baerg Hall on October 27, 2021
October is ADHD Awareness Month. Patients may be increasingly aware of ADHD, having heard about the associated functional impairment and identifying with these stories. Treatment for adults with ADHD is effective. For best results, treatment includes both medications and Executive Function Skills support.
By Dr. Linda Uyeda and Dr. Ashley Miller on July 7, 2021
The ingredients needed to create a happy workplace also largely reflect the principles of secure attachment. Across all levels within organizations, if people do not feel “safe, seen, soothed, and secure” they are more likely to make errors, breach safety protocols, and struggle working together as a team.
By Dr. Ashley Miller and Dr. Linda Uyeda on May 12, 2021
As I started to understand that this pandemic would wear on, I had to figure out how to help my patients’ families and my own family navigate our way through this totally new reality. I drew on the science of attachment, resilience and healthy relationships to make a plan. (Please stay tuned for Article #3!)
By Dr. Linda Uyeda and Dr. Ashley Miller on March 3, 2021
(Please stay tuned for Article #2: ‘Parenting during a pandemic’. We will expand on how to nurture these secure attachments with our children.) By Dr. Linda Uyeda (biography and disclosures) and Dr. Ashley Miller (biography and disclosures) (Members of the Child and Youth Mental Health and Substance Use Community of Practice and the Working Group […]
By Dr. Joanna Cheek on August 5, 2020
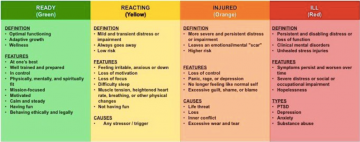
It’s not easy to train in new skills to support our mental health when the race has already begun. We are all going to cycle out of the green zone many times, regardless of our practice of self-care. We need each other right now to provide peer support to help each of us notice when we’re moving to the right of the stress continuum and pause or pace ourselves so we can complete this marathon together.
By Dr. Susan Woolhouse on February 26, 2020
My past experiences during my palliative care rotations reassured me that children could benefit from bearing witness to a loved one’s death. Why would MAID be any different? I set out to learn more about how children grieve and ways in which I could support children through the dying of a loved one seeking MAID.
By Dr. Mary V. Seeman on February 5, 2020
Fellow psychiatrists often ask whether their patients with schizophrenia are aging prematurely. They point to the fact that several of their patients seem slowed down, forgetful, fidgety, and that they garble their words and stutter. These are, of course, all side effects of antipsychotic medication.
By Dr. Dan Bilsker on January 8, 2020
It is well-known that men die on average 3-4 years before women – but why? We identified three main factors contributing to Years of Life Lost by men compared to women: cardiovascular disease, suicide, and motor vehicle accidents. As a psychologist, I was intrigued by the substantial contribution of suicide.
By Dr. Tahmeena Ali on August 21, 2019
I now ask all patients, young and old, new to my practice and established for years, male and female, to complete an ACEs questionnaire in my clinic. I garner a new level of respect for my patients’ resilience and for the ongoing turmoil many of my young patients face. I make finding supports for these young vulnerable patients one of my top priorities—as important as a referral to a specialist or for diagnostic imaging.
By Dr. Joanna Cheek on May 8, 2019
View personality disorder symptoms as important treatment targets in themselves. Be curious about each patient’s story, validate PD symptoms as coping mechanisms, focus on collaborative problem solving, set proactive regular visits, and also be mindful of your own emotional reactions providing compassion and empathy while setting clear boundaries.
By Nichole Fairbrother on March 20, 2019
Unwanted, intrusive thoughts of accidental harm to one’s infant are reported by 100% of new mothers, and unwanted, intrusive thoughts of intentionally harming one’s infant are reported by 50% of new mothers. Ask specifically about unwanted, intrusive thoughts of infant-related harm. Educate pregnant women and normalize the occurrence of the thoughts. Reassure women that, in the absence of any additional risk factors for child abuse, disclosure of these thoughts will not result in any action on the part of the care provider/physician.
By Michelle C. Danda, RN, BN on October 10, 2018
I realized that engagement is paramount when working with an ambivalent patient, because the change that they want to make is often important in their life, even if the clinician views it as a problem behavior. Motivational interviewing education has been shown to improve patient alliance and treatment adherence.
By Dr. Carol-Ann Saari on September 5, 2018
In the general population, approximately 75% of Canadians will report having experienced an adverse and potentially traumatic experience in their lifetime, with 9.2% meeting criteria for PTSD. We have to become trauma informed. Trauma informed practice (TIP) is a way of providing services that recognizes the need for physical and emotional safety, choice and control in decisions affecting one’s treatment and an environment where patients do not experience further traumatization.
By Dr. Maia Love on July 4, 2018
Defining yourself as a person first, and your role as a professional second, has benefits in preventing burnout and creating more personal energy. Put your own oxygen mask on first.
By Dr. Andrew Howard, Tyler Schwaiger, Dr. Noah Silverberg, and Dr. Will Panenka on May 2, 2018
Rest might increase symptoms and recovery time following concussion or mild traumatic brain injury. Inactivity has been associated with physical deconditioning, social isolation, discouragement about recovery, and reactive anxiety and depression. Early mobilization and graded exercise programs can reduce post-concussive symptoms and recovery time.
By Dr. Anne Antrim on July 18, 2017
The current definition of Autism Spectrum Disorder has 2 criteria: “persistent impairment in reciprocal social communication and social interactions” AND “restricted, repetitive patterns of behavior”. The symptoms must be present from early childhood, but may not manifest till the social demands exceed the capacity of the child to respond.
By Dr. Randall White on May 10, 2017
When psychiatric patients are treated in an emergency department, they are often hypervigilant, manic, or otherwise in an excited, agitated state. The current standard of care to manage acute agitation in adults is using an antipsychotic medication and a benzodiazepine, often loxapine or haloperidol and lorazepam.
By Dr. Dan Bilsker on March 8, 2017
Treatment plan should specifically target psychological problems that are barriers to occupational, relationship or emotional function, rather than broadly defined issues. Being able to return to work is a substantial benefit for the individual: staying at home for an extended time is damaging to the individual’s self-esteem, coping ability and psychological health. Practice “positive psychology”, emphasizing the outcomes that determine the meaning and success of one’s life and focus on individual’s strengths to reach goals.
By Dr. Alisa Lipson on September 28, 2016
As a general pediatrician, I see many children whose behaviour and/or development is not emerging as expected. A diagnosis such as autism or learning disability may be the obvious explanation; but frequently it is not so straightforward. Parents come armed with questions about ‘processing disorders’ and and they expect their MD to be knowledgeable.
By Dr. Clara van Karnebeek and Dr. Sylvia Stockler on July 29, 2015
Affecting 2-3% of Canadians, intellectual disability (ID) is a lifelong, devastating condition defined by deficits in cognitive functioning (IQ<70) and adaptive skills. It is called global developmental disability (GDD) in children less than 5 years of age; it is defined as deficits in 2 or more developmental domains. In Canada, approximately 7,600-11,500 children are born annually with GDD. Identification of GDD or ID in children is the essential first step and often a task for the primary care practitioner.
By Dr. Randall White on July 8, 2015
Simple use of a self-rated symptom checklist can double the odds of response to antidepressant medication in primary-care patients.
By Dr. Daniel Dodek on March 18, 2015
Mental health problems including anxiety, depression and stress make up a large proportion of a typical day in primary care medicine. They also contribute a huge comorbid burden in specialty care. These conditions all require an intense amount of time to help and manage patients.
By Dr. Alexander Chapman on January 6, 2015
Often, self-injury is managed and treated in the context of therapy work with a psychologist or psychiatrist. Family physicians, however, are in an excellent position to be first responders, to offer helpful suggestions, and to help refer the patient to appropriate care.
By Dr. Alisa Lipson on September 30, 2014
Autism rare? Not so now. The current prevalence is a staggering 1 in 68, about four times as common as type 1 diabetes, with a male to female ratio of 5:1.


















Recent Comments